We care about our patients and we know sometimes making the proper choice for your dental treatment can present some difficulties. Therefore we made an effort in putting together a small video library to help our patients get familiarize with common dental procedures and make the right choice, after consulting with your dentist.
The ADA Patient Education Library provides the most popular topics in dentistry that will help you better maintain your dental health. Select an article or video below to get started now.
Dental x-rays provide important information about your dental health. They are used to create images called radiographs.
Your dentist uses the images to see your jawbones, the roots of your teeth, teeth under your gums and the areas between teeth.
X-ray images help your dentist find problems that cannot be easily seen during your regular dental exam. Treating dental problems at an early stage can help stop them from getting worse and prevent pain. It also can help you avoid more serious health problems.
Dental x-rays use very low levels of radiation, much less than that used in other medical imaging. They are done only when needed to make a diagnosis or to help your dentist make a treatment plan for you. Your dentist will use your health history, present oral health and risk for disease to decide if x-rays are necessary.
If you change dentists, you may be able to have copies of your x-ray images sent from your last dental office to your new one. If not, your new dentist may need to take x-rays to get a full picture of your oral health. This will also help your dentist create a baseline to see how your oral health may change over time.
Dental practices take steps to protect you from radiation, including:
Many dental offices use digital dental x-ray images. Benefits of digital x-rays include:
Tell your dentist if you are or might be pregnant. Current guidelines say it’s better for a pregnant woman to have necessary dental x-rays rather than put off having them at a later date. This is because dental disease that is not treated during pregnancy can lead to problems for you and your unborn baby.
Radiation therapy to treat head or neck cancer may increase your risk of tooth decay. The dose of radiation from regular dental x-rays is very small compared to the dose used to treat cancer. It’s important to have x-ray exams as needed to find dental problems at an early stage and treat them before they get worse.
Federal and state governments have regulations about the proper, safe and effective use of x-rays in dentistry. Your dentist follows these rules to keep you safe. If you have questions about x-rays, talk with your dentist or dental staff.
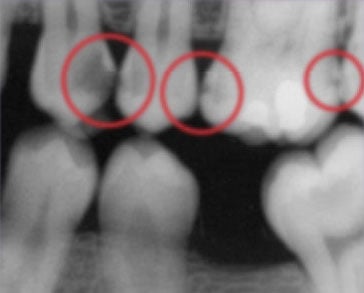
This bitewing shows several areas of decay between (and within) teeth.

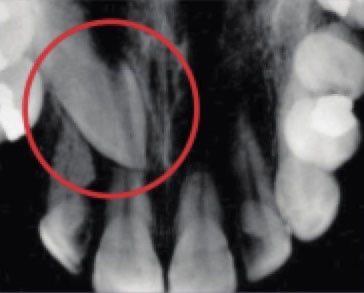
This periapical x-ray shows the top of a molar unable to reach the surface (impacted).
This occlusal x-ray shows a tooth that hasnot yet reached the surface (unerupted).
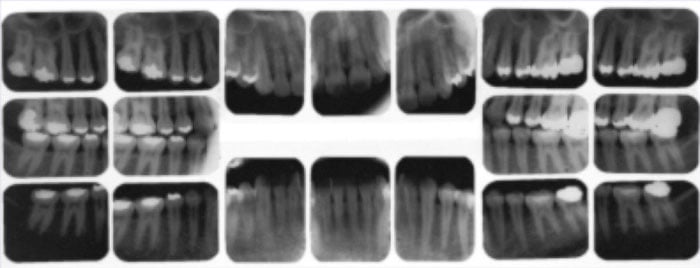
Complete series x-ray.
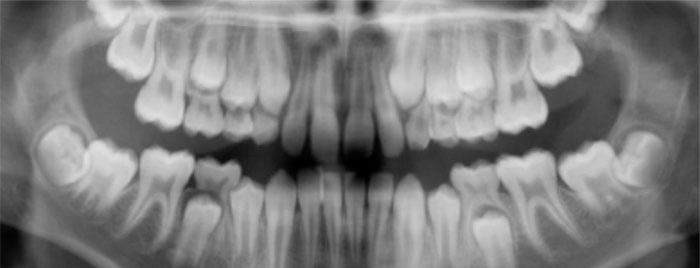
This panoramic x-ray shows baby teeth as well as the developing permanent teeth that have not yet reached the surface.
A tooth that is cracked can be painful. It also can lead to disease of the tooth.
It can be hard for you to tell if a tooth is cracked. If you have pain, you may not be able to tell which tooth hurts or even whether the pain comes from the top or bottom of your mouth. Cracks may be invisible to the eye and may not even show on an x-ray. And sometimes you won’t have any pain or sensitivity at all; your dentist will discover it during your exam.
If you are having symptoms, you can help your dentist find the cracked tooth by sharing some information:
A tooth may crack for many reasons, such as:
Pulp is the soft tissue inside the center of your tooth and contains nerves and blood vessels. If the crack reaches the pulp, your tooth may be sensitive to hot and cold. Sometimes, a crack in the enamel of your tooth goes all the way down to the nerve pulp. This type of cracked tooth may hurt when you bite down or when you stop biting. The crack may be too small to see but is large enough for the pulp inside your tooth to become irritated.
When your tooth is cracked, the pulp sometimes becomes infected. If this happens, treatment to remove the pulp, also known as a root canal, may be needed to save your tooth.

A small crack in the tooth
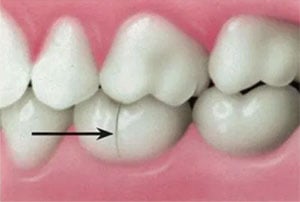
Crack widens when teeth bite down
Treatment depends on the size, location and direction of the crack, as well as your symptoms. It is possible that your dentist will recommend no treatment at all, since tiny cracks are common and usually do not cause problems. You and your dentist can talk about the types of treatments for your tooth and decide on the treatment that is right for you.
Regular dental checkups are important, because they let your dentist find and treat problems at an early stage. A cracked tooth can become a bigger problem if left untreated. If you think you may have a cracked tooth, visit your dentist.
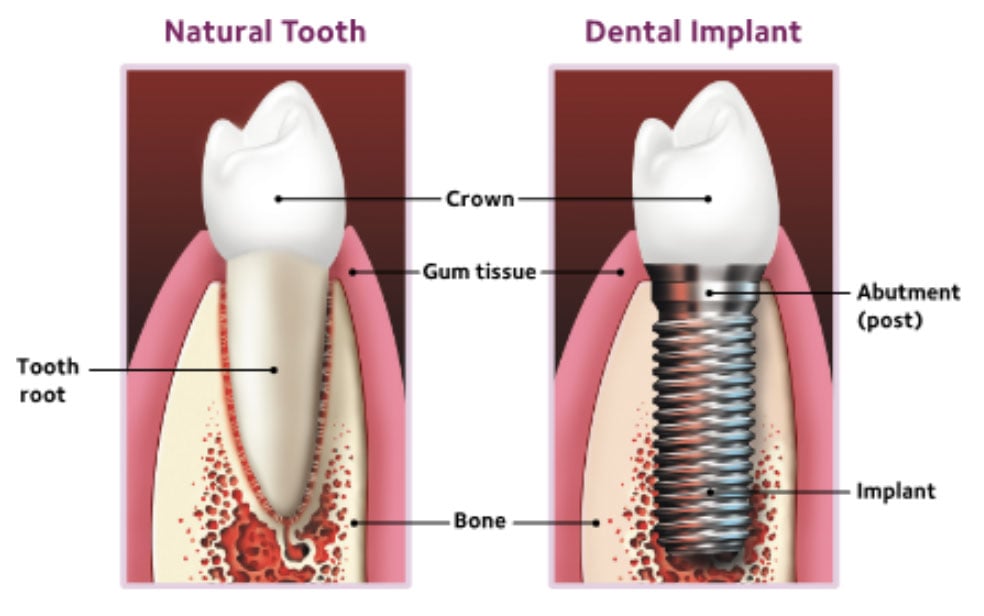
Dental implants are posts surgically placed into the upper or lower jawbone. They replace one or more teeth that are next to each other. Implants are an effective way to replace missing natural teeth. When teeth are lost because of disease or an accident, dental implants may be a good option. You may want to choose dental implants if:
People may choose implants to replace a single tooth, more than one tooth, or to support a full set of dentures.
Dental implants are made of titanium (a strong, lightweight metal) and other materials. Millions of implants are placed by dentists every year in the United States, which makes them a very common and popular option for replacing teeth.

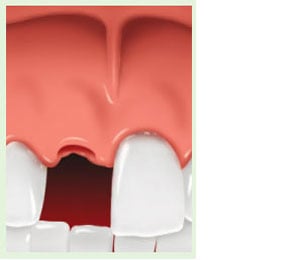
Missing tooth

Missing tooth replaced by a dental implant
Implants offer firm support to natural teeth and have many benefits, including these:
A single tooth implant replaces the missing tooth’s roots. It is a stand-alone unit and does not involve treating the teeth next to it.
If you are missing one or more teeth, there are many reasons why you should replace them:
You may not like how the gap looks when you smile.
Missing teeth may affect how you speak.
A missing back tooth (molar) can make it harder to chew.
When a tooth is lost and not replaced, the teeth around it can shift. Shifting teeth can affect how you bite and chew.
Bone loss may occur in the area of the missing tooth or teeth. This may cause the remaining teeth to become loose over time.
Loss of teeth and bone can make your face sag. You may look older.
An implant-supported bridge replaces the lost natural teeth and some of the tooth roots when more than one tooth is missing. Unlike traditional bridges, an implant-supported bridge does not need support from the teeth next to it.
Missing teeth
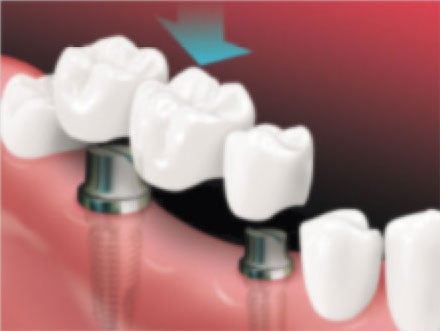
A bridge is placed on implants
After the bridge is placed
If you are missing all of your teeth, an implant-supported denture can replace the missing teeth and some of the tooth roots.

Before

With Implants

After
Because the bone in your jaw actually grows around the implants, an implant-supported denture tends to be comfortable and stable. This allows you to bite and chew naturally.
Treatment will depend on your personal case and can take only one day, several months, or somewhere in between. Discuss with your dentist which type of implant is best for you. Then, they can create a treatment plan for you.
Implant placement usually involves 3 main steps:
Replacement teeth usually take some time to make. In the meantime, your dentist may give you a temporary crown, bridge or denture. This will help you eat and speak normally until your permanent replacement teeth are ready.
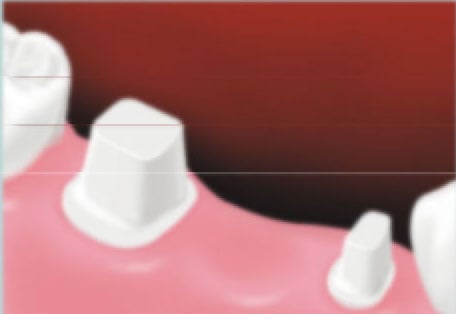
Before implant
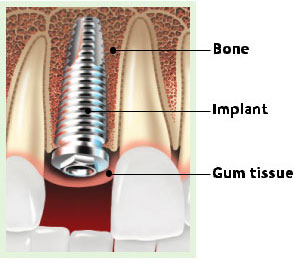
The implant is placed in the jaw. Bone and tissues grow around the implant
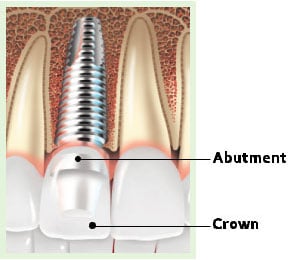
A crown is placed on the implant. The crown may be connected to the implant by an abutment
Implants are not an option for everyone. You should be in good health and/or cleared by your doctor before scheduling any implant surgery.
If your dentist does recommend implant treatment, consistent and good oral hygiene is very important for the success of the implant. You must spend time caring for the implant and making sure the area around it is very clean. If not, it increases your risk for infection, which can weaken the bone and tissues that are needed to support the implant.
You should talk about implant treatment carefully with your dentist. Dental implant treatment can take longer and cost more than other replacement options, but they are often a good value because they can last a lifetime.
Regular dental visits and putting in the time to take care of your implant are key to the long-term success of your implant. Your dentist will set up a program to help you keep your implant and natural teeth healthy.
Your dentist also will suggest a home-care routine that meets your needs. It will include brushing twice a day and cleaning between your teeth at least once a day. You also may be told to use a special toothbrush or mouthrinse to help prevent cavities and gum disease.

Flossing picks, sticks or brushes can help clean around implants
Floss threader
If you are missing a tooth, there are many reasons to replace it:
Effects of a missing tooth
Position of teeth immediately after a tooth is lost.
If the tooth is not replaced, other teeth can drift out of position and change the bite.
Nothing replaces your natural teeth, but dental implants can come close. Implants have been used for many years. They are man-made “anchors” that look like screws and are made of titanium and other materials that are compatible with the human body. The single tooth implant is placed by surgery in the upper or lower jaw, where it replaces your missing tooth’s root(s).
An implant looks and acts like a natural tooth. It fits securely even when you chew and speak. A single tooth implant does not involve treatment to your other teeth. Plus, it may also help you keep a good level of bone around your teeth.
The way implants are placed depends on your anatomy or bone structure, the type of implant, and the tooth being replaced. Some implants require 2 or 3 appointments and can take up to a year to complete. Other implants can have a temporary crown placed on the same day. You and your dentist can discuss which type is best for you.
Most implants involve 3 or 4 basic steps:
Your dentist surgically places the implant into your jawbone. There may be some swelling and/or tenderness after the surgery, so pain medication may be prescribed to ease the discomfort. Your dentist may recommend a diet of soft foods during the healing process.
What makes an implant so strong is that the bone actually grows around it and holds it in place. This process is called osseointegration (OSS-eo-in-tee-GRAY-shun) and takes time. Some people might need to wait until the implant is completely integrated before a permanent replacement tooth can be attached to the implant. This can take several months. Other people can have the implant and a temporary replacement tooth placed all in one visit. The length of the healing process depends on location of the replacement tooth and the type of implant being used.
For a single tooth implant, your dentist custom-makes a new tooth for you, called a dental crown. It is based on a size, shape, and color that will blend with your other teeth. Once completed, the man-made tooth is attached to the implant post or abutment.
Your dentist can help you decide if you can get a dental implant. In most cases, you are a good candidate if:
You’ll need to make sure the area around the implant is especially clean. Your dentist may recommend that you use a special toothbrush, called an interproximal brush, or a mouthrinse to help prevent gum problems.
You should also choose oral care products with the American Dental Association Seal of Acceptance. A product that displays the ADA Seal is your assurance that it has met ADA standards for safety and effectiveness. All of these accepted products will help ensure the area around your implant remains healthy.
Veneers are thin shells of dental material that are custom-made to fit your teeth. They look like natural teeth, but without imperfections. Veneers can be used to correct a wide range of dental issues, such as:
Veneers are made from either ceramic or composite resin. Your dentist will help you choose the material that is best for you. Each type of veneer has its own benefits.

A porcelain veneer is placed

After placement
A ceramic veneer is a thin shell that is custom-made to fit on the front surface of your tooth.
A composite resin veneer is made from a tooth-colored filling material that is bonded to the tooth.
As with all your dental care, discuss your expectations and treatment options with your dentist. Regular dental visits are important for keeping your teeth and gums healthy.
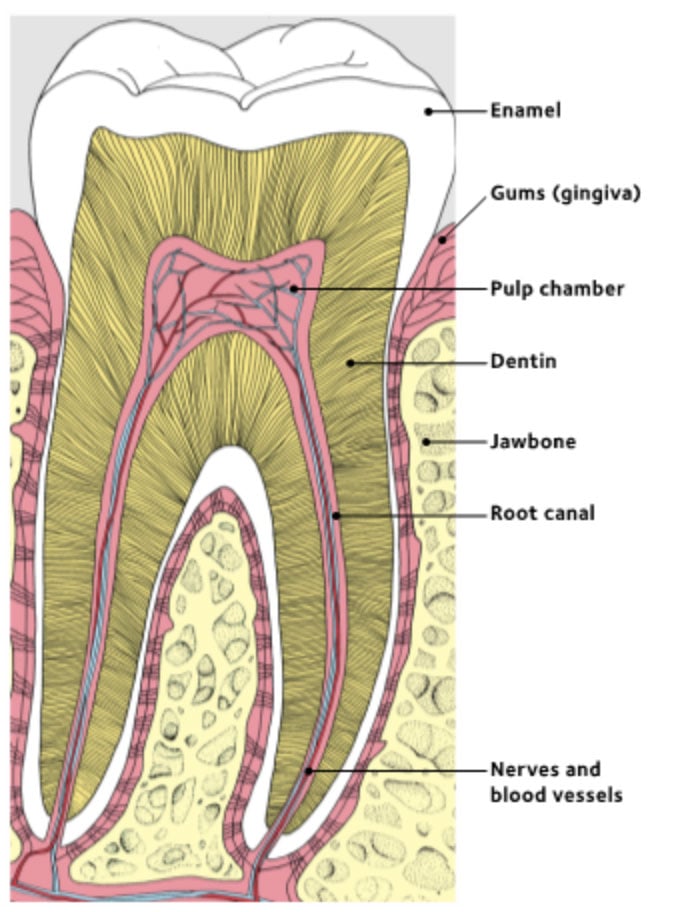
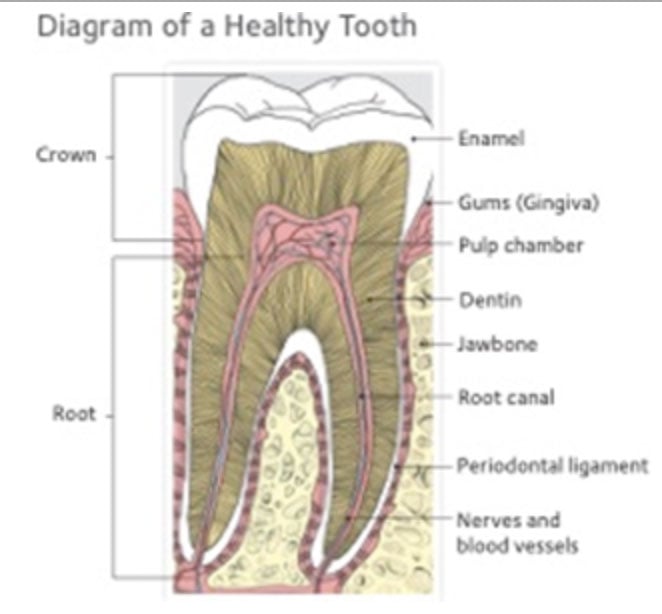
Your teeth have a hard, outer layer, called enamel (e-NAM-uhl); a middle layer, called dentin; and a center, which contains the nerves and blood vessels, known as the pulp chamber.
Tooth decay can affect each layer of your tooth, and the more layers that are affected, the worse the damage.
Your teeth are covered by a sticky film of bacteria called plaque (pronounced PLACK). When plaque is left on your teeth, the bacteria in the plaque use sugar in food and drinks to make acid. This acid attacks your tooth enamel. Eventually, your enamel can break down from these acids and cavities can start to form. Once a cavity forms, it can’t be reversed. Cavities can only be treated and repaired by a dentist, usually with a filling.
If tooth decay is not treated, you may feel pain, the infection can spread to other parts of your mouth, and you may even lose teeth. People with tooth pain may have trouble eating and sleeping and may miss days of work or school.
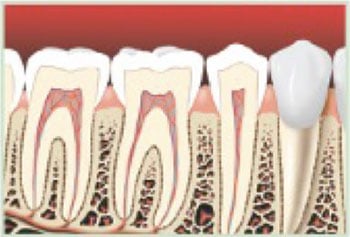
Healthy teeth and roots without signs of decay
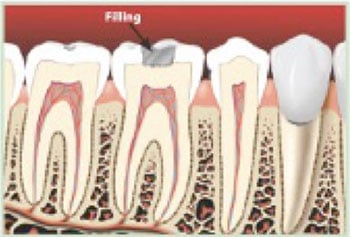
Early decay may not be easy for you to notice, especially if it forms in an area that can’t be seen like under a filling
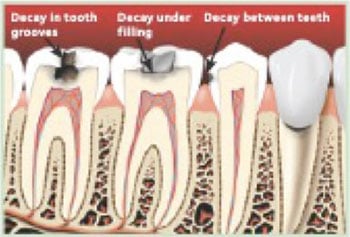
Decay under the surface may be larger than it looks from the outside
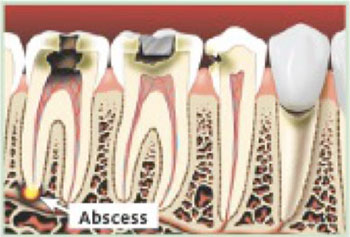
If not treated, tooth decay can cause an abcess and can lead to serious infections
You may not notice any signs or symptoms at all, so it’s important to see your dentist regularly. He or she will examine your teeth and take x-rays if needed.
Tooth decay often occurs between teeth and in the grooves of back teeth, where bits of food collect. Toothbrush bristles often do not get into these grooves. Back teeth are also harder to keep clean because they are not as easy to reach. Another place decay can form is at the tooth root. Cavities there may go below the gumline.
Your risk may increase if you:
The bacteria that cause tooth decay can also be passed from one mouth to another by kissing, sharing a cup or spoon or anything else that carries saliva. For this reason, you should not share toothbrushes with anyone.
Treatment depends on the size and location of the decay. Your dentist can explain what treatment is best, depending on how much the decay there is.
It is faster, easier and less expensive to prevent tooth decay than to repair or replace a decayed tooth.
Periodontal (perry-o-DON-tal) disease is an infection that affects the tissues and bone that support your teeth. It is also called gum disease.
Periodontal disease can become a very serious problem if it’s not treated early.
This booklet is your complete guide to gum disease and can help you learn about:
A surprisingly wide variety of bacteria live in your mouth. This is normal. When certain types of bacteria outgrow the others, you may begin to develop gum disease.
Plaque is a sticky film that is always on your teeth. When plaque is left on your teeth and gums, it can harden. Hardened plaque is also called tartar (TAR-ter). Bacteria that live in the plaque can make your gums red, puffy and swollen. Tartar on your teeth makes it hard for you to keep your teeth and gums clean on your own.
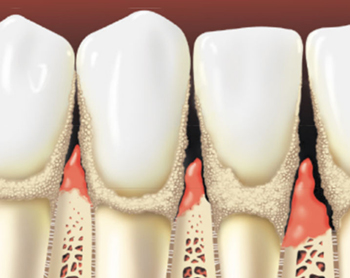
When your gums are healthy, your gum tissues tightly hug each of your teeth. When you have gum disease, your gums pull away from your teeth and may become red, puffy and swollen. Spaces called pockets can form, and these pockets collect more bacteria. If the infected pockets are not treated, the disease will get worse.
As the gum disease gets worse, the tissues and bones that support your teeth can become damaged. Over time, your teeth may fall out or need to be removed.

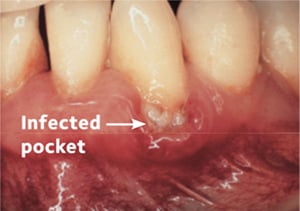
Periodontal disease can get worse if it’s left untreated. It can lead to serious infection, bone loss and you may even lose teeth.
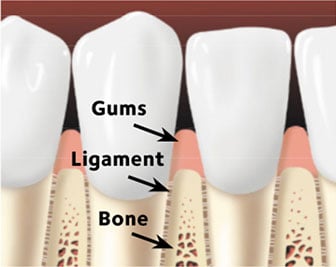
Your teeth are held in place by gums, bone and connective tissues. Your gums hug your teeth tightly and there is little or no buildup of plaque and tartar on them.

The bacteria in plaque make your gums red, tender and swollen. Your gums might bleed at this stage. You also can have gingivitis and not notice any of these signs. Gum disease at this stage is usually reversible and can be treated by a dentist or dental hygienist during a regular cleaning and with daily brushing and flossing.

In time, as plaque and tartar build up where your teeth and gums meet, the gum tissues and bone around your teeth begin to break down. Periodontitis affects about 42% of adults over age 30 in the United States.
Your teeth may become loose and fall out or need to be removed by your dentist. This stage is very serious and may require surgical treatment.
Anyone can get periodontal disease, but some things can raise your chances of getting it. Factors that can increase your risk of getting
periodontal disease include:
Periodontal disease has been linked to some other diseases. People with diabetes or heart disease are more likely to get gum disease.
It is important to talk to your dentist if you suffer from any long-term health problem.
You may notice one or some of these warning signs, or you may not notice any warning signs at all. Sometimes the only way to know for sure is by getting regular dental checkups. That way, if you do have gum disease it can be caught and treated early.
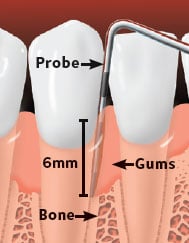
At your dental appointment, your dentist will use an instrument called a periodontal probe to gently measure how deep the pockets are around each of your teeth. When your teeth are healthy, the pocket should be no deeper than 3 millimeters. Typically, the worse the disease, the deeper the pocket. This means the bacteria have more room to grow and cause serious damage to your gums and bone, loosening your teeth. Very deep pockets are a sign of advanced periodontal disease.

Periodontal probe of healthy gums.
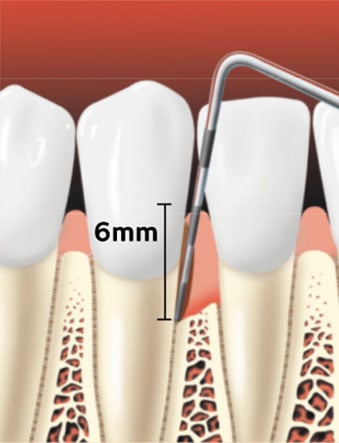
Periodontal probe showing a pocket forming between the tooth root and the gums.
Dental x-rays can be taken to check for the amount of bone that is supporting your teeth. If low bone levels are spotted, it could be a sign of damage from gum disease.

Healthy gums have bone that supports the teeth.
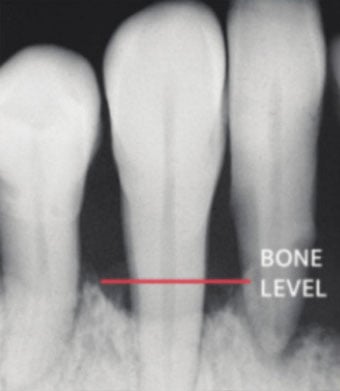
Gum disease can create bone loss.
Your periodontal disease treatment will depend on several factors, including your personal health history and the stage of your gum disease.
Your dentist may also refer you to a periodontist — a dentist who specializes in the treatment of gum disease. A periodontist is well versed in the surgical treatment of gum disease.
In the very early stages — when it is gingivitis — you may just need a professional cleaning from your dental team. They can also give you tips on how you can keep your teeth and gums healthy.
If your gum disease is beyond gingivitis, you may need a special deep cleaning called scaling (SCAY-ling) and root planing (PLAY-ning). This treatment may be done over more than one visit, depending on your diagnosis.
During scaling, your dentist or dental hygienist will carefully remove plaque and tartar down to the bottom of each pocket.
The next step is root planing, which is cleaning and smoothing your tooth’s root surfaces. Smoothing the surfaces helps your gums heal and reattach to the tooth, shrinking the pocket depth.
You will need to schedule another dental visit within a few weeks or months after your scaling and root planing treatment has been completed. At this visit, your dentist or hygienist will check your gums to see how they have healed. They will measure the periodontal pockets again. Scaling and root planing may be only a first step in periodontal treatment.

Scaling removes plaque and tartar from below the gumline.

Root planing smothes the tooth root and helps the gums reattach to the tooth.

Healed pocket after treatment.
Sometimes, scaling and root planing isn’t enough treatment on its own. If the pockets do not heal enough after scaling and root planing, gum surgery may be needed. Surgery can help repair bone and gum damage or help to shrink pocket depth and make it easier for you to keep your teeth clean.
One type of procedure is flap surgery, which allows your dentist to remove plaque and tartar from hard-to-reach areas below the gum. A small incision is made in the gums and the gum tissue is pulled back to allow the area to be cleaned. Then, your gums are stitched into place to tightly hug your teeth.
Probe shows pockets due to gum disease. Gums are inflamed and bone loss has occured.

The bone is contoured and any remaining tartar is removed.

Healed site after periodontal surgery.
If bone has been damaged or lost by gum disease, you may need surgery to rebuild or reshape the bone in your mouth. This kind of surgery is called a bone graft.
A bone graft holds your loose teeth in place and natural or synthetic bone is placed to help support regrowth of bone.
Your dentist may place a membrane layer at the surgical area to help your gums stay in place while the tooth root reattaches to the supporting bone tissues. This is called guided tissue regeneration.
To help you heal after surgery, your dentist may apply a protective dressing over your teeth and gums and recommend or prescribe a medicated mouthrinse. You may also be given a prescription to treat infection or for pain relief.

Diseased tissue is removed from the pocket. In some cases, the bone may be reshaped.

Bone has been reshaped.

Grafting material is placed over the bone.

After the healing period.
Once your gum disease is brought under control, it is very important that you get dental care on a consistent basis. The type of professional cleanings recommended after your treatment are called periodontal maintenance care. These cleanings are more extensive than the standard cleaning and will help you keep your gums healthy.
You will need to clean your teeth and gums every day at home, but that is not enough to control your gum disease. Professional care is also needed to help make sure that your mouth continues to heal and get healthy. Your periodontal maintenance involves cleanings that are deeper than a normal cleaning in the dental office. These cleanings lower the amount of plaque bacteria so inflammation gets better, pockets shrink and gums become healthier. Periodontal maintenance appointments are typically every 3 to 4 months, depending on your condition.
Once your gums are healthy, periodontal maintenance cleanings can help keep them infection-free. Your dentist will determine a maintenance schedule based on your clinical evaluations.
You will need to see your dentist more often than other people. The pockets and other issues from your gum disease will make it harder for you to clean plaque from your teeth.
Your dentist will talk to you about a treatment plan that works best for you, and he or she will recommend a maintenance care schedule that is based on your personal case. Over time, fewer appointments may be necessary.
It’s important to follow your periodontal maintenance care. You have a better chance of keeping your teeth if you do. Your gum disease may get worse if you don’t!
You may also need special medications that can help control the infection or help your gums heal. The medicine could be a pill, a special mouthrinse or a medication that your dentist places right into the pocket after you have a deep cleaning.
It is very important that you brush and floss every day — especially if you are healing
from gum disease.
 Look for the American Dental Association Seal of Acceptance on all of your dental care products. The ADA Seal means these products have met ADA standards for safety and effectiveness.
Look for the American Dental Association Seal of Acceptance on all of your dental care products. The ADA Seal means these products have met ADA standards for safety and effectiveness.
Remember, it’s possible that you may not feel any pain or see any signs that your gum disease is getting worse.
You may have sensitive teeth and gums after your treatment. Sensitive or sore teeth and gums may make you want to skip cleaning the treated areas in your mouth — but don’t! It is important that you keep brushing your teeth gently and flossing to remove plaque. If you don’t remove the plaque, your gum disease may get worse and you may increase your risk of cavities.
Ask your dentist or dental hygienist about special toothpastes or other treatments that can lower your tooth sensitivity.
Don’t use tobacco! If you smoke, chew or dip tobacco, it is very important you quit. Using tobacco in any form slows down your healing and raises your chances of getting gum disease again or it getting worse if you already have it. Talk to your dentist or doctor about ways you can quit.
Be sure to check your benefits plan when you are planning your treatment with your dental office. However, treatment should be decided by you and your dentist and not by your benefits plan.
If your treatment plan is not fully covered by insurance, ask if your dental office has a payment plan to cover the rest of the amount. Keep in mind that having treatment now may cost less than having to replace one or more teeth lost to gum disease later on.
In general, it costs much less to keep your teeth and gums healthy than to wait until you have a problem.
These healthy habits can help:
Every patient is different, so talk to your dentist about the information in this guide and what it means for your personal treatment plan.
Your teeth are meant to last a lifetime. If your tooth becomes diseased or injured, it can often be saved through root canal therapy.
Your tooth may look like one solid piece, but it has many layers. There are two main parts of your tooth: the crown and the root. The crown is the part of the tooth you can see. The root is the part of the tooth below the gumline in the jaw bone.
The inside of the crown contains the pulp chamber, which continues toward the tip of the root in what is called the root canal. In each root, there may be one or more root canals. The root canals contain the dental pulp, which is made up of nerves and blood vessels and extends all the way to the tip of each root. When the pulp tissue becomes infected or inflamed, treatment is needed. Root canal therapy is a procedure that removes injured or infected dental pulp from the canal.
All of these can allow bacteria to enter the pulp and cause infection and inflammation.
The infection and inflammation in the pulp can spread to the tissues around the root of the tooth. This can cause pain and swelling and can lead to a pus-filled sac called an abscess. But, even if there is no pain, bacteria from the infection can damage the bone that holds the tooth in your jaw.
Without root canal therapy, the infection and damage will continue and your tooth most likely will need to be removed.
Endodontics (en-do-DON-tics) is the branch of dentistry that specializes in treating diseases of or injuries to the dental pulp. Endodontists are dentists who specialize in treating these diseases and injuries. Your dentist may refer you to an endodontist to perform your root canal therapy.
Root canal therapy may involve one or more dental visits.
Your dentist or endodontist will perform the necessary steps to save your tooth:
For your root canal treatment to be successful, it is very important that you follow instructions from your dental team and attend all of your follow-up appointments.
Most patients have very little or mild discomfort after treatment, which can usually be controlled with over-the-counter medication. Talk to your dentist about options for pain relief.
If you feel severe pain or pressure for more than a few days, have visible swelling or if your bite feels uneven, contact your dentist or endodontist.
After your root canal procedure, avoid biting down or chewing with the affected tooth until it is fully restored with a crown. Make sure to continue brushing twice daily and cleaning between your teeth once a day to keep the area clean and free from infection.
When properly restored and maintained, a tooth with a root canal filling can last for many years. But, like any other tooth, it can become decayed or fractured or the tissue around it can get gum disease. Professional cleanings and regular dental exams will help keep your mouth healthy — whether you’ve had root canal therapy or not.
Tooth decay can cause an abscess.
The decay is removed and an opening is made through the crown of the tooth into the pulp chamber.
The pulp tissue inside the root is removed, and the root canals are cleaned, shaped and disinfected.
The root canals and pulp chamber are filled. If there is not enough tooth to hold the restoration, a metal rod (post) may be placed in the root canal to help retain the core (filling) material, which supports the restoration (crown).
The crown of the tooth is then restored. If bone is lost due to infection at the root tip, this will heal over several months after the root canal is cleaned and sealed.
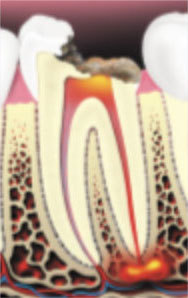
Tooth decay can cause an abcess.
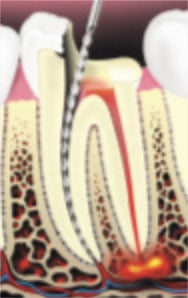
The decay is removed and an opening is made throuh the crown of the tooth into the pulp chamber.

The pulp tissue inside the root is removed, and the root canals are cleaned, shaped and disinfected.

The root canals and pulp chamber is filled.

If there is not enough tooth to hold the restoration, a metal rod (post) may be placed in the root canal to help retain the core (filing) material, which supports the restoration (crown).
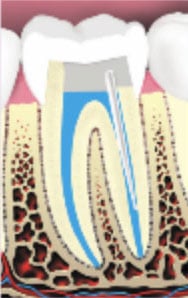
The crown of the tooth is then restored. If the bone is lost due to infection at the root tip, this will heal over several months after the root canal is cleaned and sealed.
If you’re missing one or more teeth, you may be all too aware of their importance to your looks and overall health. Your teeth are designed to work together to help you chew, speak, and smile. Replacing a missing tooth (or teeth) helps to make sure that all of your teeth continue to work together. Plus, it helps protect your remaining teeth.
Here are some problems that can happen if you choose to not replace a missing tooth:
Replacement teeth should last for years at a time, so it’s important to choose a treatment that’s right for you. Depending on your needs, this section discusses 3 options your dentist may suggest:
Removable Partial Dentures
Fixed Bridges
Implants
Position of teeth immediately after a tooth is lost.
If the tooth is not replaced, other teeth can drift out of position and change the bite.
When teeth are lost and not replaced, the face looks older. The lips appear thin and flattened. The chin moves forward and upward and appears pointed.
Also, the mouth loses some of its shape, and the lip line straightens. Pouches become pronounced on either side of the lower jaw. Cracks and sores may form at the corners
of the mouth.
A removable partial denture usually has replacement teeth fixed to a metal or acrylic (plastic) base that matches the color of your gums. The acrylic base may cover a framework made of several durable materials. Partial dentures often have some form of clasp that attaches to your natural teeth and can easily be taken out of your mouth for cleaning or storing while you sleep.
Your dentist may also recommend crowns, or “caps,” on your natural teeth. Crowns may improve the way a removable partial denture fits your mouth.
They are usually less expensive than fixed bridges or implants or when replacing multiple teeth.
They don’t require teeth next to the space to be prepared.
They are usually easier to repair than fixed bridges.
They can be removed for cleaning.
They can be less stable than other choices.
They can break or be lost.
They may take longer to get used to wearing because it could take several appointments for your dentist to achieve the right fit.
Some people are embarrassed to take out their teeth at night and for cleaning.
They may need more frequent replacement than implants or a fixed bridge.
A fixed bridge is a restoration that fills the space where one or more teeth have been lost. A fixed bridge is permanently bonded or cemented into place — this means that only a dentist can remove it.
They can look, feel and function like natural teeth.
They don’t require removal for cleaning.
They may cost less than implants.
They affect the teeth next to the missing tooth — once they are prepared for placement of the bridge, they will permanently lose their natural look and shape.
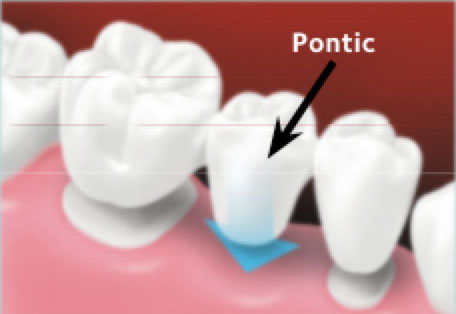
They may require extra effort to clean under the replacement tooth (called the pontic).
They are likely to be more expensive than a removable partial denture.
Placing a bridge usually takes more than one dental visit. On your first visit, your dentist prepares the teeth on either side of the gap. The bridge will later be attached to these teeth.
Implants are posts (metal “roots”) that are surgically placed in your upper or lower jaw, where they function as a sturdy anchor for replacement teeth. They are made of titanium (a strong, lightweight metal) and other materials that are accepted by your body. Many people choose implants to replace a single tooth, several teeth, or to support a full set of dentures.
A dental implant may be right for you if you:
Most people find that an implant is a good replacement for their missing tooth because it’s secure and stable.
A tooth implant is a surgical procedure, so it’s not an option for everyone. You may be a good candidate for an implant if you:
If you have a chronic illness like diabetes or high blood pressure, you may not be a good candidate for implants because it can take you longer to heal after surgery. Drinking alcohol and using tobacco or e-cigarettes can also slow healing. Your dentist can help you decide if implant treatment is a good option for you.
An implant is most similar to a natural tooth and often feels more comfortable.
Nearby teeth remain unchanged and do not have to be involved in the placement procedure.
They are a good value because they can last a lifetime with good care.
They may help prevent shrinkage of the jawbone from tooth loss.
They may fit better and be more comfortable than removable partial dentures.
They require a surgical procedure to place them.
Implant placement may take longer and may require more dental visits than other options.
They may cost more than other treatments.
Talk to your dentist. You can get answers to your questions and together you can decide which option will work best for you: removable partial dentures, fixed bridges, or implants.
Here is a list of words that were used in this brochure. Your dentist may refer to these terms when he or she is discussing your treatment plan with you.
Attachment tooth/teeth: The prepared teeth on either side of the gap that hold the fixed bridge in place.
Bridge: A tooth replacement option that fills the space where one or more teeth are missing by permanently connecting a replacement tooth or teeth into place.
Crown: A “cap” that is either placed over attachment teeth as part of a fixed bridge or placed over an implant itself to serve as a new tooth replacement.
Partial Denture: A tooth replacement option in which the replacement teeth are fixed to a metal or acrylic base. It has clasps that attach to your natural teeth to hold the denture in place and is removed daily to be cleaned and while sleeping.
Implant: A tooth replacement option in which a metal post is surgically placed in the upper or lower jaw bone and acts as a support for a replacement tooth or teeth.
Sometimes, teeth need to be removed due to decay, disease, or trauma. When you get a tooth “pulled,” it’s called an extraction.
It’s natural that changes will occur in your mouth after the procedure. Here are some general guidelines to help promote healing, prevent complications, and make you more comfortable while you recover.
Follow all instructions from your dental team. This will help make sure that your mouth heals properly after your tooth is removed. These instructions will also help to lower your risk of having any problems while your mouth heals.
Your dentist may place a gauze pack on the extraction site to limit bleeding. This will also help a blood clot to form, which is necessary for normal healing. This gauze pack should be left in place for 30 to 45 minutes after you leave the dentist’s office.
Do not chew on the pack. There may be some bleeding or oozing after the pack is removed.
If so, here’s what to do:
To help reduce swelling and pain:
If you cannot reach your dentist, go to a hospital emergency room.
The blood clot that forms in the tooth socket is an important part of the normal healing process. You should avoid doing things that might disturb the clot. If the blood clot is disturbed and breaks down, you can get a dry socket. Dry sockets can be extremely painful. To lower your risk of a dry socket, be very careful to not do anything that can disturb the clot.
For the first 24 hours, do not suck, spit, slurp, or any other action that creates suction in your mouth and puts pressure on your blood clot. This means:
Wisdom teeth are the four permanent (adult) teeth at the very back of your mouth on the top and bottom. They are the last permanent teeth to appear. Wisdom teeth get their name because they usually come in between the ages of 17–21, around the age when a person gains maturity and wisdom. Most other permanent teeth come in a few years earlier, by age 13.
Sometimes wisdom teeth do not have enough room to come in, or they are in the wrong position. They may come in sideways or at a slant, pushing against the teeth next to them (Figure). These wisdom teeth are called “impacted” and may have to be removed so that they don’t cause future problems.
Regular dental visits allow your dentist to track the growth and condition of all of your teeth. After doing an oral exam and taking X-rays, your dentist can look at your wisdom teeth and talk to you about whether they should be removed. Wisdom teeth extraction, or removal, may require surgery.
Your dentist will examine your wisdom teeth and may recommend having them removed so they don’t cause future problems.
A general dentist can perform wisdom tooth extractions. But, if your dentist sees a need for any special care, you may be referred to an oral and maxillofacial (max-UH-lo-FAY-shul) surgeon. This is a dentist who specializes in surgery of the hard and soft tissues of the mouth, including the removal of impacted wisdom teeth. If your dentist refers you to a specialist, the two will work together to provide you with the best care.
In some cases, there may be complications after treatment. It is possible to get “dry sockets.” Dry sockets can develop when the blood clot that forms over your socket is displaced, leaving bone and nerves exposed. Smoking can increase the risk for complications and delay healing. Follow your dentist’s instructions carefully to reduce the risk for complications.
Not everyone’s teeth develop on the same schedule. See your dentist regularly so he or she can monitor the growth of your wisdom teeth.
Some people think that pain after wisdom teeth removal can only be tackled with prescription medicines. But that’s not true. Studies show that a combination of ibuprofen and acetaminophen—both common pain relievers you can buy off the shelf under many brand names—work just as well as prescription medicines without the side effects like the potential for addiction. Talk to your dentist about options for pain relief.
If you use tobacco in any form, it is important to quit. Smoking and vaping can cause problems with your healing process. Ask your dentist or physician for information about ways to quit.
Periodontal Disease Is Also Known as Gum Disease
Periodontal (perry-o-DON-tal) disease is a bacterial infection leading to inflammation of the tissues that support your teeth. It’s also called gum disease.
When your gums are healthy, your gum tissues tightly hug each of your teeth. When you have gum disease, your gums pull away from your teeth. As the gum disease gets worse, the soft tissues and bone that support your teeth are damaged.
Over time, your teeth may become loose, fall out or may need to be removed. Treating gum disease in the early stages is very important because it can help prevent tooth loss.
This brochure talks about scaling (SCAY-ling) and root planing (PLAY-ning) – a type of deep cleaning treatment that your dentist may recommend for treating your gum disease.
Causes of Gum Disease
Plaque is a sticky film in which bacteria grow that is always on your teeth. Dental plaque begins to re-form after a teeth cleaning. When left undisturbed, the plaque hardens into tartar (TAR-ter), sometimes call dental calculus. Your body may react to the bacteria in plaque, resulting in inflammation of the gum tissue and bone that support your teeth.
When your gums are red, puffy and swollen, they can start to pull away from your teeth. Spaces called periodontal pockets start to form between your gums and teeth. Bacteria collect
in these pockets.
As the bacteria collect in the pockets, your gum disease will get worse. The bacteria in the pockets produce toxins. Your body’s response to the toxins causes the soft tissues and bone around your teeth to break down.
Checking for Gum Disease
Your dentist or hygienist uses an instrument called a periodontal probe to measure how deep the pockets are around each tooth. When your teeth are healthy, the pocket is usually 3 millimeters (mm) deep or less.
Typically, the worse the disease, the deeper the pocket. This means bacteria have more room to grow and cause serious damage to your gums and bone, loosening your teeth. Very deep pockets are a sign of advanced periodontal disease.
Dental x-rays are another tool used to check your teeth and the supporting bone. Bone loss can be
a sign of damage from gum disease.
All dentists are trained to detect, treat and monitor gum disease. But, your dentist may send you to a periodontist (perry-o-DON-tist) – a dentist who specializes in the treatment of gum disease.
Your gum disease treatment will depend on several factors, including your personal health history and the stage of your gum disease.
The first step in treating gum disease usually involves scaling and root planing. This treatment may be done over more than one visit, depending on your diagnosis.
Scaling: Your dentist or hygienist removes plaque and tartar down to the bottom of each pocket.
Root Planing: Then, the root surfaces of your teeth are smoothed, or “planed,” to allow the gum tissue to heal and reattach to the teeth.
Your dentist may recommend certain medicines to help control infection and discomfort or to aid healing. After your treatment, your dentist may give you medicine in the form of pills, a mouth rinse or medicated material placed directly into the pocket to help control infection.
Scaling and root planing is not the same as a regular cleaning! This treatment is a deeper cleaning that focuses on getting your infection and inflammation under control. Be sure to follow all of the recommendations of your dentist, or your gum disease could get worse.
Tobacco use in any form makes gum disease worse. This includes smoking, vaping, chewing or dipping – all of which can cause problems for your healing process and make it harder for your gum disease to improve. Talk with your dentist or physician about ways to quit.
You will have a follow-up visit with your dentist
You will need to schedule another dental visit within a few weeks or months after your scaling and root planing treatment has been completed. At this visit, your dentist or hygienist will check your gums to see how they have healed. They will measure the periodontal pockets again. Scaling and root planing may be only a first step in periodontal treatment.
Once your periodontal treatment is complete, your dentist may recommend that you have more frequent checkups and cleanings. This is to help keep your gums as healthy as possible.
Regular dental visits and maintenance care are important to keep your gum disease under control. Depending on your personal case, your appointments may alternate between your general dentist and your periodontist.
Keep up with your oral hygiene at home!
Usually, tooth decay and gum disease occur because teeth and gums are not properly cleaned.
Your teeth are covered with a sticky film of bacteria called plaque. Plaque builds up after you eat and when you sleep. The bacteria in plaque turn the sugar in foods and drinks into acids. These acids attack the enamel, your tooth’s hard, outer layer. Repeated attacks can cause the enamel to break down and lead to tooth decay and cavities.
If plaque stays on your teeth, it can cause problems like these:
Tartar: Over time, plaque hardens into tartar (also called calculus). Tartar can build up on the gum line — this is where your tooth meets your gums. It can give bacteria a place to grow without being disturbed. If the tartar is not removed, your gum disease can get worse and cause tooth loss.
Cavity: A hole in your tooth called a cavity can form when tooth decay gets through your enamel. The cavity can continue to spread deeper into the layers of your tooth. Cavities can form on any tooth and in any place on your tooth. If tooth decay and cavities are not treated, you may feel pain, the infection can spread to other parts of your mouth, and you may even lose teeth.
Gum disease: Plaque can also irritate your gums, making them swell or bleed. This is called gingivitis (jin-ji-VY-tis). Gingivitis is the early stage of gum disease. If gum disease isn’t treated, it can cause your gums to pull away from your teeth. Pockets or spaces can form between your teeth and gums. These pockets can become infected. In advanced stages of gum disease, bone loss occurs and teeth may become loose, fall out, or have to be removed.
Brush with a fluoride (FLOOR-eyed) toothpaste to help prevent tooth decay. Fluoride is a naturally occurring mineral that helps make tooth enamel stronger. There is more than one way to brush your teeth, so it’s a good idea to ask your dentist or hygienist which way works best for you.
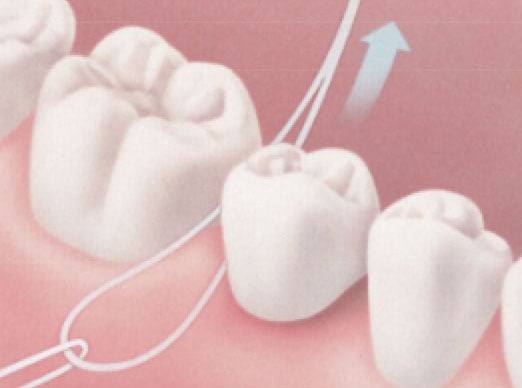
Even if you brush twice a day, there are places your toothbrush bristles can’t reach. Flossing removes plaque and food particles from between teeth and under the gum line. Your dentist or hygienist can show you the right way to floss. It may feel clumsy at first, but don’t give up! It takes time to get the hang of it.
If you haven’t been flossing, you may have sore or bleeding gums for the first few days that you floss. This should stop once the plaque is broken up and the bacteria are removed. If bleeding does not stop, see your dentist or hygienist.
Traditional string floss may not be the right method for you — and that’s okay! The best way to clean between your teeth is whichever way you will actually do every day. These types of between-the-teeth cleaners are also called interdental cleaners.
Here some other options:
It doesn’t take a lot of pressure to brush your teeth the right way. If you brush too hard then you may irritate your gums. This can cause them to pull away (recede) and expose the tooth’s root to bacteria in your mouth.
Flossing is an important part of your oral care routine. It is one of the best ways to keep your teeth and gums healthy. However, it takes a little practice to floss well. Here are some tips to help.
There are many kinds of between-the-teeth cleaners to choose from. Talk to your dentist or hygienist about which type will work the best for you.
Brushing your teeth twice a day with a fluoride (FLOOR-eyed) toothpaste is important. But, toothbrush bristles cannot reach the spaces between teeth. These spaces trap bits of food and plaque, a sticky film of decay-causing bacteria. Dental floss or other between-the-teeth cleaners can help keep these tooth surfaces plaque-free and healthy. Also, eating a healthy diet, limiting snacks, and having regular dental checkups will help you keep your smile healthy for years to come.
Start by choosing a brand of floss that shows the American Dental Association Seal of Acceptance. This means the product has met the ADA’s standards for safety and effectiveness. Your dental office may also recommend certain products for your oral health needs.
Here are some tips for flossing effectively. It may feel clumsy or awkward at first, but don’t give up! It takes a little time to get the hang of it.





Brush your teeth twice a day and for two minutes each time. Use a toothpaste that contains fluoride (FLOOR-eyed), a natural mineral that helps make your teeth stronger. It’s also important to clean your teeth with floss or another between-the-teeth cleaner every day. This helps remove bits of food and plaque from between the teeth and under the gum line that
a toothbrush can’t reach.
Choose a soft-bristled toothbrush in a size and shape that fits your mouth comfortably. Replace your toothbrush every three months, or sooner if the bristles are worn or frayed. Worn toothbrushes won’t clean teeth properly.
Both manual and powered toothbrushes are effective at removing plaque. If you have hand, arm or shoulder problems that limit movement, a powered toothbrush may be easier for you to use.
Supervise teeth brushing for children up to age 6—make sure they use the right amount of toothpaste and spit the toothpaste out. Begin brushing children’s teeth as soon as the first tooth comes in and until the age of 3 years, using a smear of toothpaste the size of a grain of rice. After age 3, use a pea-sized amount.

For children under three years old.

For children three to six years old.
When choosing a toothbrush, floss and fluoride toothpaste, look for products that show the American Dental Association Seal of Acceptance. This means that the product meets the ADA’s standards for safety and effectiveness.
Talk to your dentist or dental hygienist about the best way to brush your teeth.
Here are a few tips to help you start a good routine:

Place your toothbrush against your gums at a 45-degree angle. Move the brush back and forth gently and in short strokes, about as wide as each of your teeth.

Brush the outer tooth surfaces, keeping the toothbrush at an angle to the gums.

Brush the inner tooth surfaces.
Brush the chewing surfaces.

Use the top part of the brush to clean the inside surface of the top and bottom front teeth. Use a gentle up-and-down motion.
Eating a healthy diet, limiting snacks and visiting your dentist regularly will help you keep your smile healthy for years to come.
A bridge is a custom-made replacement tooth or teeth that fill the space where one or more teeth are missing.
The bridge permanently restores your bite and helps keep the natural shape of your face.
This brochure reviews the types of non-removable bridges available and the steps involved in placing your bridge. Your dentist can recommend which type of bridge is best for you based on your specific needs.
A missing tooth is a serious matter. Teeth are made to work together to help you chew, speak and smile. When you lose a tooth, the nearby teeth may shift and become crooked. This may make it harder to speak or chew. A missing tooth in the lower jaw may cause a tooth in your upper jaw to shift down into that space, meaning your teeth will no longer be even or in a straight line. This can affect your bite and place more stress on your teeth and jaw joints, possibly causing pain and damage.
Teeth that have tipped or drifted are also harder to clean. This can increase the risk for tooth decay and gum disease.
Missing teeth can lead to bone loss, which can cause neighboring teeth to become loose and can lead to facial collapse. If that happens, it may change the way the jawbone supports the lips and cheeks. Over time, this can make your face look older.

Position of teeth immediately after a tooth is lost.

If the tooth is not replaced, other teeth can drift out of position and change the bite.
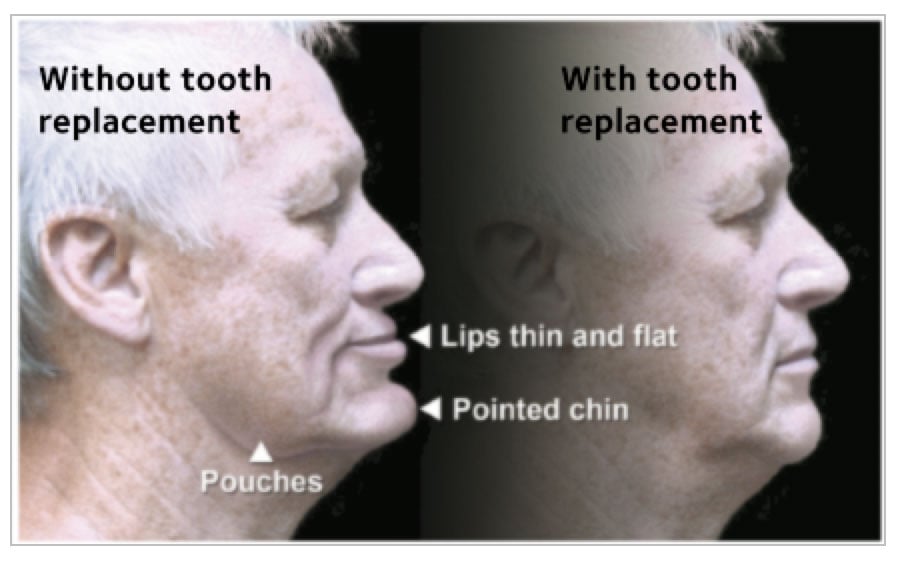
When teeth are lost and not replaced, the face looks older. The lips appear thin and flattened. The chin moves forward and upward and appears pointed.
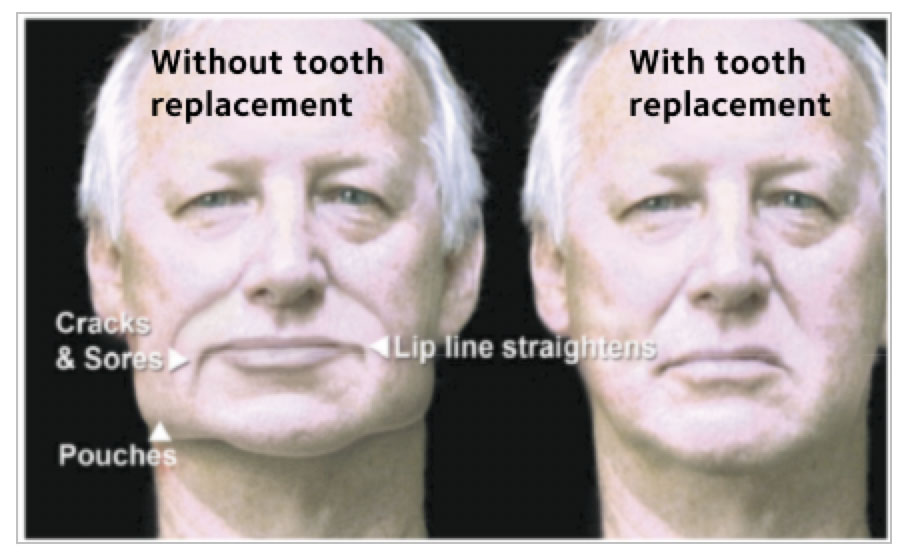
Also, the mouth loses some of its shape, and the lip line straightens. Pouches become pronounced on either side of the lower jaw. Cracks and sores may form at the corners of the mouth.
To place a fixed bridge, your dentist uses an existing natural tooth or teeth to help hold your bridge in place. Fixed bridges are cemented in place and only a dentist can remove them. This makes them feel stable and very similar to your natural teeth.
An artificial tooth, called a pontic, takes the place of the missing tooth. The pontic is secured by one or more crowns, which are bonded to the teeth on either side of the missing tooth.
Placing a bridge takes several dental visits. Depending on your needs, one or more teeth may be prepared to hold the bridge. Let’s use the example of a bridge supported by two teeth:
An implant-supported bridge is a bridge that is attached to one or more metal posts that are surgically implanted into your jawbone. The posts act like the roots of natural teeth. The bridge, which has replacement teeth mounted on a tooth-colored base, attaches to these metal posts. A key benefit of an implant-supported bridge is that it doesn’t need support from the surrounding teeth.
An implant-supported bridge requires surgery to place the post into the bone. Candidates for dental implants should be in good general health and have enough bone to support an implant.
Implants may be placed in one day or may require multiple visits depending on the existence of a previous infection, the availability of bone to hold the implant and your dentist’s treatment plan.
Bridges are made from metal, ceramics or a combination of the two. Your dentist will talk with you about the materials that are best for you and your mouth.

Missing tooth
To replace a missing tooth with a conventional three-unit bridge, teeth next to the gap are reduced.
The custom-made bridge is placed over the prepared teeth.

After adjustments are made, the bridge is cemented into place.
Missing teeth
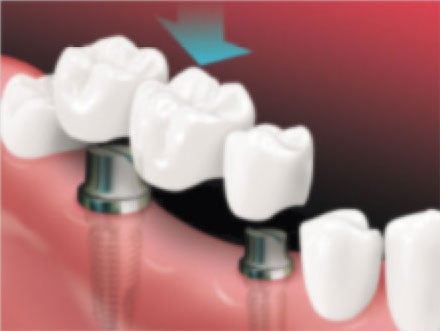
A bridge is placed on implants
After the bridge is placed
A bridge can become loose if the support teeth or the jawbone are damaged by dental disease. Follow these tips for good oral health:
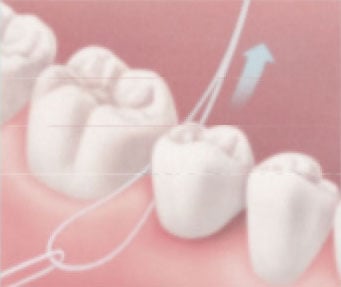
Using a floss threader, insert floss under the bridge.
Gently rub the side of each tooth next to the bridge with the floss, cleaning under the gum, too.
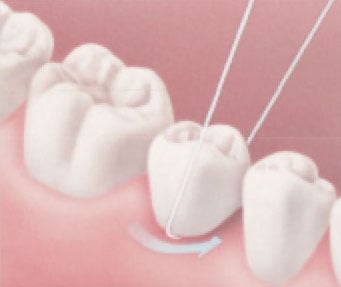
Rub the floss from side to side along the underside of the pontic.
A crown restores a damaged or missing tooth to its normal shape, size and function. A crown can protect the tooth or improve the way it looks.
Your dentist may recommend a crown to:
Crowns can be made from several types of materials. Metal alloys, ceramics, porcelain, porcelain fused to metal or composite resin may be used. When a crown is made, the material often is tooth colored to blend in with your natural teeth.
You want your crown to look natural and fit comfortably in your mouth. To decide which material to use for your crown, you and your dentist will consider many factors, such as:
Costs and insurance should also be discussed and considered. After you and your dentist have looked at these factors, you might want to talk about your personal preference.
It usually takes two dental visits to complete the treatment. When a crown is placed over a natural tooth, several steps are involved:

Before crown: Worn filling with decay under filling
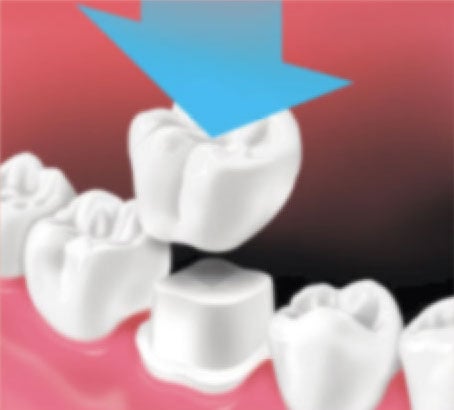
Crown is placed over prepared tooth

After crown placement

Like natural teeth, crowns can break. And, the tooth under the crown can still get cavities. To prevent cavities or damage to your crown:
Periodontal (perry-o-DON-tal) disease is an infection in your gums that may cause them to bleed or become swollen and sore. It can lead to the loss of the bone that supports your teeth, which can cause tooth loss. Periodontal disease, also called gum disease, is common and can affect people at any age.
The mildest form of periodontal disease is called gingivitis (jin-ji-VY-tis). It makes gums red and swollen and they may bleed easily when you brush. The good news is that gingivitis can be reversed. Sometimes all it takes is better oral care at home and more professional cleanings.
The more advanced form of the disease is called periodontitis (perry-o-don-TIE-tis). It results in more swelling and redness in the gums. In advanced stages, it can also cause the tissue and bone that hold your teeth in place to break down.
You can have periodontal disease without pain or other symptoms. This is one of the reasons why it is important to visit the dentist regularly.
Regular dental visits allow your dentist to detect and treat problems in their early stages before they have a chance to get worse.
Some people with periodontal disease have few or no warning signs. If you notice any of these signs, see your dentist:
Periodontal disease is caused by plaque (pronounced PLACK), a sticky film that forms on your teeth. Plaque contains bacteria that can lead to periodontal disease.
Healthy gum tissue hugs your teeth tightly. But swollen and irritated gums can pull away from the teeth and form spaces called pockets. These pockets collect more plaque bacteria. If the infected pockets are not treated, the disease will get worse. Bone and other tissues that support teeth can be damaged. Over time, teeth may fall out or need to be removed.
If plaque stays on your teeth, it hardens into a rough substance called tartar. Tartar can trap plaque along and under the gum line, which can increase the chances of developing gum disease. Tartar can only be removed when teeth are cleaned by a dental professional.
You can prevent the buildup of tartar with a good oral care routine at home. You can remove plaque by brushing your teeth twice a day and cleaning between your teeth daily. Keeping your teeth and gums healthy helps prevent tooth loss.

Normal, healthy gums

Severe periodontal disease
Your dentist checks for problems by looking at the color and firmness of your gums. He or she also uses a tool called a periodontal probe to gently measure how deep the pockets are between your teeth and gums. When your teeth are healthy, the pockets are usually 3 millimeters (mm) deep or less.
Typically, the worse the disease, the deeper the pocket. This means the bacteria have more room to grow and cause serious damage to your gums and bone, loosening your teeth. Very deep pockets are a sign of advanced periodontal disease.
During your visit, dental x-rays may be taken to check the amount of bone supporting your teeth. Your dentist may also check how well your teeth fit together.
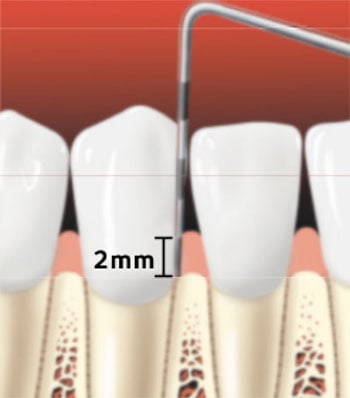
Periodontal probe of healthy gums
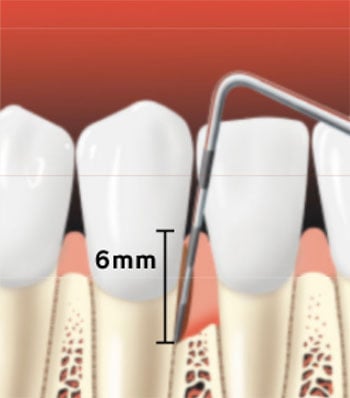
Periodontal probe showing a pocket forming between the tooth root and the gums
If you have periodontitis, your dentist may suggest a deep cleaning treatment called scaling (SKAY-ling) and root planing (PLAY-ning). He or she carefully removes plaque and tartar down to the bottom of each periodontal pocket. Your dentist will also smooth your tooth’s root surfaces to allow the gum tissue to heal and reattach to your tooth. This treatment often takes more than one visit.
To control infection, sometimes antibiotics can be placed directly in the pocket after scaling and root planing. Your dentist may also prescribe a mouthrinse to help the area heal.
All dentists are taught to detect and treat periodontal disease. Sometimes your dentist may refer you to a periodontist. This is a dentist who specializes in treating periodontal disease. Periodontists are well-versed in the surgical treatment of the disease.
Periodontal disease will not go away by itself. Preventing and treating the disease in the early stages are the best ways to keep your smile healthy and avoid tooth loss. If you have periodontal disease, follow your dentist’s recommendations for treatment and follow-up care.
This article explains how fluoride helps keep teeth strong and healthy. Cavities that are not treated can cause pain, loss of teeth, and spread of infection. The good news is you can prevent most cavities with good dental care and fluoride.
Fluoride (FLOOR-eyed) is a natural mineral in all water sources — even oceans and lakes. Fluoride can prevent cavities in children and adults. Cavities can be caused by sugar and acid in our food and drinks. Fluoride helps protect tooth enamel (e-NAM-uhl), the hard outer surface of your teeth, from the acid attacks that cause cavities. It also helps repair weakened enamel before cavities form and reverses signs of decay.
Teeth get fluoride in two ways:
To prevent cavities, it is best to get a little bit of fluoride both ways.
Fluoride that is swallowed usually comes from tap water. In some parts of the U.S., the tap water naturally has justx the right amount of fluoride. In other places, the tap water does not have enough fluoride. So, some cities and towns add fluoride to the tap water. This is called water fluoridation.
Many communities in the U.S. adjust the level of fluoride in their public water systems to 0.7 milligrams of fluoride per liter of water (0.7 mg/L). This is the recommended level in drinking water for good oral health. Almost 75% of the people in the U.S. have public water systems that are fluoridated.
When fluoride is put onto the surface of your teeth, it is called topical fluoride. Fluoride toothpastes and mouth rinses sold in stores are one way for your teeth to get topical fluoride. Also, your dentist can apply a fluoride gel or varnish to your teeth.
Your home water filter system might remove fluoride from the water. Reverse osmosis and distillation systems can remove fluoride. However, filters that come in pitchers or attach to your faucet generally do not remove a lot of fluoride. Check with the maker of the product to learn if the filter or system removes fluoride from your drinking water.
Most bottled waters do not have the levels of fluoride needed to help prevent cavities. If you drink bottled water often, you may be missing the benefits of fluoridation. To learn about the fluoride level in the water, check the label. If it is not listed, you should contact the manufacturer.
More than 70 years of study and experience have shown that water fluoridation is safe. Fluoridation of community water is supported by leading health organizations, including the American Dental Association (ADA), the Centers for Disease Control and Prevention (CDC), the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the World Health Organization (WHO).
To find out if the tap water in your area contains fluoride at a level that can help prevent cavities, ask your dentist. You also can contact your community’s water supplier. If you have a private water well, the Environmental Protection Agency (EPA) recommends you test your water every year for safety. These water tests can include fluoride levels.
Begin brushing the teeth of your children under the age 3 years as soon as teeth begin to come into the mouth. Use no more than a grain-of-rice-sized amount of fluoride toothpaste on the brush. Watch children to make sure they don’t swallow the toothpaste.
Put no more than a pea-sized amount of fluoride toothpaste on the toothbrush. Help your child brush and teach him or her to spit out the toothpaste and not swallow it.
Fluoride mouth rinses are not recommended for children under 6 years. Parents should keep an eye on children under 6 years when they use any dental product with fluoride. More fluoride is not always better. These products should be stored out of the reach of young children.

For children under three years old.

For children three to six years old.
Have more questions? Visit MouthHealthy.org fluoride for the latest information about fluoride and fluoridation.
Not everyone lives in an area with fluoridated water. For those people, fluoride is available in other forms. If your community’s water does not have fluoride, talk to your dentist or physician about your family’s fluoride needs.
Fluoride pills, drops and lozenges are for children between 6 months and 16 years old who live in areas with little or no fluoride in the water and are at high risk of tooth decay. For best results, these fluoride products should be used every day until the child is 16 years old. Ask your child’s dentist or physician about your child’s fluoride needs. Supplements are available only by prescription.
Fluoride toothpastes and mouth rinses with the ADA Seal of Acceptance help prevent cavities in children and adults. When you shop for dental products, look for the ADA Seal so you know that a product is safe and effective. You and your children should brush your teeth twice a day using a toothpaste that contains fluoride.

If you skip cleaning between your teeth because you have trouble flossing or you simply don’t like to do it, then you are putting your mouth at risk for problems like cavities or gum disease.
Traditional string floss may not be the right method for you — and that’s okay! The best way to clean between your teeth is whichever way you will actually stick to doing every day.
Here are 3 other ways to clean between your teeth that can be just as effective as floss:
If you have trouble holding floss with your fingers, these pre-threaded flossers have an easier-to-hold handle that can help you reach in between your teeth. These are also convenient for travel and to clean between your teeth when you’re on the go.
These brushes help “sweep” away plaque and food that your regular toothbrush can’t reach. Also known as interdental brushes, they are ideal for keeping orthodontic work like braces clean, too.
Dental picks are made of wood or plastic and are specially designed to remove plaque and help to stimulate blood flow in your gums. (Note: these are not the same as regular toothpicks!)
Powered cleaners work much like a powered toothbrush. They may use string floss or a gentle yet powerful stream of water to remove bits of food and plaque from between your teeth and below the gum line. Many have timers and different levels of intensity — all at the push of a button.
Powered cleaners are ideal if you have problems with your grip, if you wear braces, or if you have had other treatments like implant-supported dentures or bridges.
No matter which way you decide to clean between your teeth, selecting products that display the ADA Seal of Acceptance is your sign that they have been tested and proven to work as they say they do.
Products with the ADA Seal take the guesswork out of selecting products that can help keep your mouth healthy.
Everybody’s oral care needs are different; the best way to clean between your teeth is the one you will actually do every day! Your dental team can help you decide which method will set you up for success.
Mouth and throat cancers can be deadly diseases. As recently as 2019, there were 53,000 new cases of mouth and throat cancer diagnosed and about 10,000 deaths from these cancers. Men are more than twice as likely to develop mouth and throat cancers as women.
Finding cancer early is important. Treatment may be more successful with mouth and throat cancers that are found early. Your dentist can check for these cancers every time you visit, so this is one more reason to see your dentist regularly.
This page will tell you some ways to lower your risk for mouth and throat cancer. By watching for the signs and symptoms listed here, you are more likely to find the cancer earlier if you do have it.
Check your mouth in the mirror each day when you brush and floss. If there are any changes in your mouth or neck, or if you notice any of these signs or symptoms, contact your dentist.
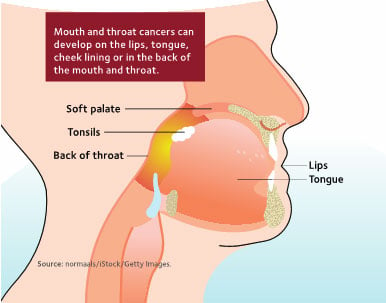
Be aware of any changes in your mouth or throat.
Anyone can get cancer. There are some factors that you can control—such as using any form of tobacco or heavy alcohol consumption—which increase your risk of getting mouth or throat cancer. Below is more information about factors that can affect your chance of developing these cancers.
When you quit using tobacco, your risk of developing mouth and throat cancers goes down.
During a dental exam, your dentist may check your face, neck and mouth for lumps, red or white patches and sore areas that do not heal. Your dentist can check for signs of mouth or throat cancers visually, manually or with a combination of these methods.
Be sure to tell your dentist if you notice any changes in your mouth or neck. If signs of cancer are found early, treatment may be more successful. If you have any concerns about mouth and throat cancer, talk with your dentist. It may help save your life.
The habit of grinding your teeth or clenching your jaw is called bruxism (BRUCKS-is-im).
Grinding is when you slide your teeth back and forth over each other. Clenching means you tightly hold your top and bottom teeth together. Bruxism is something that children and adults of any age may do.
Bruxism can happen when you are awake or while you are sleeping. You may wake yourself up with a loud grating or grinding sound. The sound may even be loud enough that other people can hear it. However, bruxism may also be silent.
Your dentist may talk to you about your symptoms and examine you for any signs that bruxism might be a problem. In some cases, he or she may refer you to a sleep medicine physician for an evaluation.
Stress and trouble sleeping are some things that may play a role in bruxism, but what is causing you to grind your teeth may not be known for sure. Children who clench or grind their teeth while sleeping are more likely to have other sleep-related issues, like snoring.
Your dentist can see if you have bruxism by checking for unusual wear spots on your teeth and looking at any related symptoms. Regular dental checkups are important to find damage in the early stages. Your dentist can help you manage bruxism and the related symptoms, as well as repair your teeth if necessary and help prevent further damage.
Treatment depends on each person’s situation. Your dentist may recommend that you wear a night guard during sleep. Night guards are custom-made by your dentist from plastic or other materials. The night guard slips over your upper or lower teeth and prevents them from touching. It protects your teeth and helps keep them from wearing down.
Your dentist may also suggest one or more other treatments, such as these:
You may need to try a few different treatments to find out what works for you. You can help manage bruxism by paying attention to the symptoms, having regular dental visits and talking with your dentist.
Bruxism that is left untreated can cause future problems such as:
Be sure to talk to your dentist if you have any signs of bruxism.
Do you have frequent headaches, earaches, tender jaw muscles or a dull, aching facial pain? Does your jaw lock or stray to one side when you open your mouth?
These aches and pains may be related to the joint in your jaw, called the temporomandibular (TEM-poro-man-DIB-u-lar) joint or “TMJ,” and the muscles that work to move the joint. These painful conditions are often called “TMD” for temporomandibular disorders.
The TMJ and muscles on each side of your jaw help open and close your mouth. These joints move in many different directions. They allow you to chew, talk, and swallow.
These 2 joints are among the most complex joints in the body. They work together in a delicate balance with muscles, ligaments, cartilage, and your jaw bones. When a problem prevents these parts from working together properly, pain may result.
A temporomandibular disorder is a condition, not a specific disease. TMD can have many different signs and symptoms, from mild to severe. Some people may have symptoms but are still able to fully function in their everyday lives. TMD appear to be more common in women. Specific symptoms may include:
This often makes it difficult to pinpoint the cause of a particular case of TMD.
Related conditions may include:
To determine how best to treat your condition, a complete evaluation is recommended.
For some patients, TMD may disappear by themselves. For others, they may come and go, or may worsen over time. TMD are often managed, rather than cured. Your general dentist may recommend treatment, or they may refer you to a physician or a dental specialist.
The success of the treatment often depends upon you and your dentist working together to find what works
best to relieve your symptoms.
Treatment may involve a series of steps. The step-by-step plan allows you to try simple treatment before moving on to more involved treatment. Experts generally recommend a “less is often best” approach to treating TMD.
In some cases, your dentist may recommend fixing an uneven bite by adjusting or reshaping some teeth. Orthodontic treatment may also be recommended.
TMD are conditions, not specific diseases. They are often managed rather than cured.
Good oral health habits not only help prevent problems during pregnancy, but they can also benefit the health of your baby.
What you eat during pregnancy affects the growth of your unborn child — including their teeth. Your baby’s teeth begin to develop between months 3 and 6 of pregnancy, so it’s important that you take in enough nutrients — especially calcium, protein, phosphorous, and vitamins A, C, and D.
You do not lose calcium from your teeth during pregnancy.
It’s a myth that this happens. The calcium your baby needs is provided by your diet and not by your teeth. So, be sure to get enough calcium in your diet by having at least 3 servings of dairy products per day. Or, your obstetrician (OB/GYN) may recommend that you take calcium pills to help make sure you are getting enough calcium.
During pregnancy, you may feel hungry between meals. While this is normal, frequent snacking on sugary foods can lead to problems with your mouth.
Your mouth is covered with a sticky film of bacteria called plaque. Plaque feeds on the sugars in your snacks. They create acid from the sugars, which attack the protective outer layer (enamel) of your teeth. This can lead to tooth decay and cavities. Also, infection that can be caused by decay can spread. Either of these problems must be treated by a dentist.
When you need a snack, choose healthy foods for you and your baby, such as raw fruits and vegetables and dairy products. Visit www.choosemyplate.gov and follow your doctor’s advice.
Pregnancy hormones can make your gum tissue more sensitive to plaque bacteria. Your gums may become red, tender, and puffy. They are likely to bleed easily when you brush your teeth. This condition is called gingivitis (jin-ja-VIE-tis) and it’s an early stage of periodontal (perry-o-DON-tal) disease. Your dentist may recommend that you have cleanings more often during your second trimester or early third trimester to help you avoid problems.
In some women, growths of tissue called “pregnancy tumors” appear on the gums, most often during the second trimester. These growths or swellings are usually found between the teeth and are believed to be related to excess plaque. They look red and raw. They usually disappear after the baby is born. Pregnancy tumors usually don’t cause problems but bleed easily, so it’s important to see your dentist.
Tell your dentist:
During pregnancy, keep seeing your dentist regularly for oral exams and teeth cleaning. If you are worried about the effects any drug, treatment, or x-ray might have on your pregnancy, discuss your concerns with your dentist and physician.
Radiation from dental x-rays is low. Current guidelines say it is riskier for you to put off necessary dental treatment than to have an x-ray when you are pregnant. This is because dental disease that isn’t treated during pregnancy can lead to problems for you and your baby.
Tell your dentist or hygienist if you are or might be pregnant. If an x-ray exam is needed, your dental team will take steps to keep the x-ray exposure as low as possible.
Your child’s baby (primary) teeth begin to appear about 6 months after birth. Most children have a full set of 20 baby teeth by age 3. Strong, healthy baby teeth help your child chew food easily, learn to speak clearly, and smile. They also help give your child’s face its shape.
You may not realize it, but your baby’s teeth can start to decay as soon as they appear in their mouth. This can happen when your baby’s teeth are in contact with sugary liquids often and for long periods. These liquids include fruit juice, soda, and even milk and formula. If decay is not treated, it can destroy the baby teeth of an infant or young child.
The good news is that your child can avoid tooth decay. Here are a few simple steps you can take to keep your child’s smile healthy:

For children under three years old.

For children three to six years old.
Think of the first dental visit as a “well-baby checkup” for your child’s teeth. This can help start a good relationship between your child and their dentist.
Did you know that your oral health is tied to your overall health? For example, periodontal (perry-oh-DON-tal) disease, also known as gum disease, is more common in people with chronic diseases like some forms of heart disease or diabetes than in people without these diseases. This brochure explains the connection between your mouth health and your overall health.
Gum disease is an infection and inflammation that affects the tissues and bone that support your teeth. Plaque (pronounced PLACK) is a sticky film of bacteria that is always on your teeth. If it is not removed with regular daily hygiene, it can make your gums red, puffy and swollen. When plaque is left on your gums and teeth, it can harden. Hardened plaque is also known as tartar. Tartar on your teeth makes it difficult for you to keep your teeth and gums clean on your own.
As gum disease gets worse, the tissues and bones that support your teeth can become damaged. Over time, your teeth may need to be removed. Gum disease happens often in adults, and if it’s not treated it can lead to tooth loss.
Gingivitis (jin-ji-VY-tis) is an early stage of gum disease. The bacteria in plaque make your gums red, tender and swollen. Your gums might also bleed at this stage. If left untreated, gingivitis can lead to more advanced stages of gum disease.
But, the good news is, gum disease at this stage is usually reversible. If it is caught early enough (when it is gingivitis), you may simply need a professional cleaning and to keep up with daily hygiene: brushing and cleaning between your teeth. Your dental team can also give you advice for improving your daily oral hygiene.
If gingivitis is not treated, it can turn into periodontitis (perry-oh-don-TIE-tis). As plaque and tartar build up where your teeth and gums meet, the gum tissues and bone around your teeth begin to break down. Periodontitis is usually not painful, but it can lead to bone loss and, in more severe cases, teeth that may need to be removed.
You may notice one or some of these warning signs, or you may not have any signs of gum disease at all. This is why it’s important to see your dentist regularly — treatment of gum disease is most successful when it’s caught early.
Diseases that lower your body’s ability to fight infections may raise your risk of gum disease. And, sometimes having gum disease is shown to raise the severity of chronic disease. While it may not be clear whether one drives the other, some of the chronic diseases that commonly occur at the same time as gum disease are:
Tell your dentist about any chronic diseases or changes in your overall health.
Many of the medications used to treat other diseases can affect your mouth by causing dry mouth. These include medications used to treat blood pressure, allergies and pain. Dry mouth can make it difficult for your saliva to help keep your mouth clean, increasing the risk of oral health problems like tooth decay and gum disease.
Make sure your dentist knows about all the medications you are taking.
Using tobacco products of any kind, like cigarettes, dip, chew and hookah can increase your risk of gum disease. The disease can also get worse the longer you use tobacco.
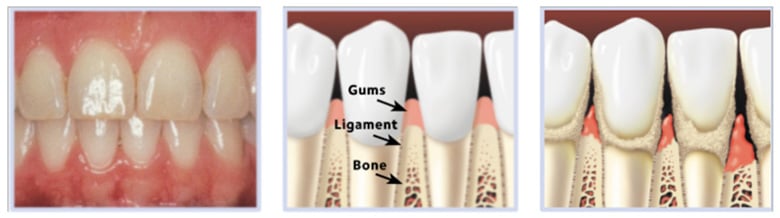
Healthygums and bone hod teeth firmly in place.
Periodontitis happens over time, as plaque builds up along the gum line. Your body responds to the toxins that the bacteria produce, which may result in the breakdown of the gum tissues and bone around your teeth.
In general, it costs much less to keep your teeth and gums healthy than to treat a problem once it happens. These healthy habits can help:
When shopping for oral health care products like toothbrushes, between-the-teeth cleaners or mouthrinses, look for the ADA Seal of Acceptance on the package. The Seal tells you that the product has met the ADA’s standards for safety and effectiveness.
For more information about taking care of your mouth and teeth, visit MouthHealthy.org, the ADA’s website just for patients.
Sucking is a natural infant reflex and necessary for feeding. Many babies begin to suck on their fingers or thumbs even before they are born. As they get older, sucking can continue for other reasons, like feeling insecure or seeking comfort. Sucking is relaxing, so it may also help them fall asleep. Young children often suck when they are tired.
Infants and young children may suck on thumbs, fingers, pacifiers or other objects while they explore new things and sensations in their world. Teething can also be a reason for sucking.
Most children stop sucking on their own between the ages of 2 and 4 years. Sucking occurs less often during this period, since children can talk and have other ways to handle new situations and deal with anxiety. Peer pressure also causes many school-aged children to stop.
If your child does not stop on their own, you should discourage the habit. However, too much pressure to quit can do more harm than good.
Thumb and finger sucking can result in problems early on for your child. The effects are especially noticeable when their adult (also called permanent) front teeth begin to come in, around age 6. Continued sucking may cause problems with the proper growth of their mouth and alignment of their teeth. It can also cause changes in the roof of their mouth.
The chance of developing dental problems depends on how often, how long, and how strongly your child sucks. Children who rest their thumbs gently in their mouths are less likely to have problems than are children who vigorously suck their thumbs.
Speech patterns such as lisping may also be affected by prolonged thumb or finger sucking. If you notice changes in the position of your child’s teeth, talk with their dentist.
Thumb sucking can cause problems as your child’s teeth and mouth develop, like crooked teeth and changes to the shape of their face and mouth.
Pacifiers can cause the same problems as thumb and finger sucking
But, pacifier use is often an easier habit to break.
Pacifier sucking can cause problems to your child’s teeth and mouth in the same way as thumb and finger sucking.
If you answered yes to any of these questions, you may be damaging your teeth. This brochure will tell you why and what you can do to keep your mouth healthy.
Certain eating patterns and food choices can lead to tooth erosion (ee-ROW-shun) and cavities. A steady diet of food and drinks that are sugary or acidic can damage your teeth. This includes soda and sports and energy drinks. It even includes seemingly healthy snacks like dried fruit or pretzels, which can be a problem if they stick to your teeth.
Here’s why:
Plaque is the sticky film of bacteria that forms on teeth. When plaque is left on your teeth, the bacteria in the plaque use the sugar left over from food and drinks to make acid. This acid attacks the hard surface of your teeth known as enamel (e-NAM-uhl). The acid can wear away your enamel, and cavities can start to form. Cavities do not go away on their own and must be treated by a dentist.
Having sugary foods or drinks many times a day allows bacteria to make acid throughout the day. This raises your risk of getting cavities. Repeated exposure to foods or drinks that are acidic raises your risk of tooth erosion (Figure 1).
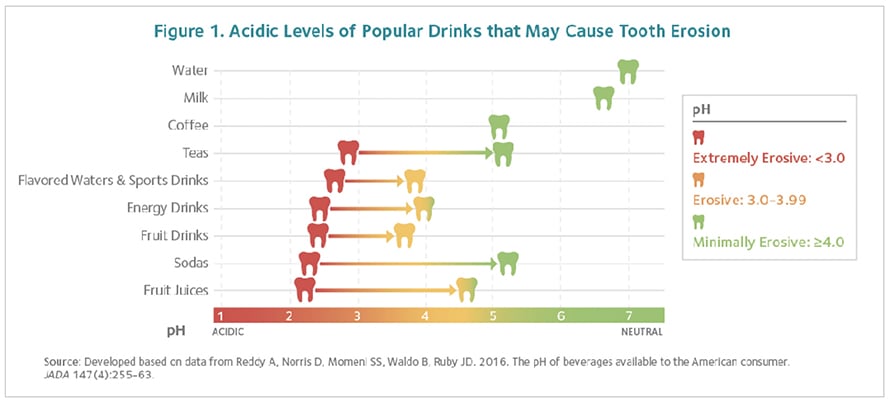
You often hear that eating a well-balanced diet reduces your risk of things like heart disease and diabetes. But, eating a healthy diet is also good for helping you avoid cavities. For teeth to be healthy, they need vitamins, protein, calcium and phosphorous — and you can get all of these from a healthy diet.
A healthy diet includes the right amounts and variety of
In addition, a healthy diet is low in added sugar, trans fats and saturated fats. MyPlate (Figure 2) shows the five food groups that are the building blocks of a healthy diet.
Many foods and drinks — like apples, oranges, bananas, carrots and milk — naturally contain sugars and also have vitamins, minerals and nutrients that your body needs to be healthy. To lower your risk of cavities, avoid foods — like candy and cookies — that contain a lot of sugar but few other nutrients.
A lot of sugar can slip by in the things you drink. Take a look at how much added sugar there is in popular beverages like fruit drinks and sodas (Figure 3).
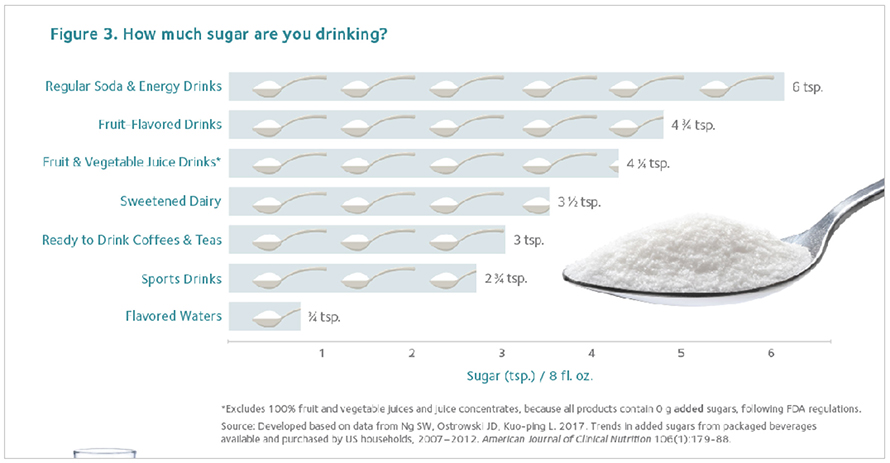
See your dentist regularly. And, brush your teeth with fluoride toothpaste twice a day.
Look for oral health products that display the ADA Seal of Acceptance. The ADA Seal is your sign that these products are tested and proven to be safe and effective in keeping your mouth healthy.
Enamel (e-NAM-ul) is the hardest outside layer of your tooth that protects a softer inner layer. Tooth erosion (ee-ROW-zhun) happens when the enamel begins to wear away, exposing the inner layer of the tooth, called dentin.
When the enamel thins out, your tooth protection is weakened and the inside layers can be exposed to more acid and bacteria. This puts you at a greater risk of having problems like sensitive teeth, decay and cavities.
Tooth erosion happens from several causes that have one thing in common — acid. If your teeth come in contact with acid on a regular basis, the acid can attack your tooth enamel and start to cause erosion. There are many ways that acid can reach your teeth, such as:
You aren’t alone. Talk to your dentist or physician about how you can get healthy. Or, call the National Eating Disorders Association Helpline and talk to someone confidentially. 1.800.931.2237.
Acids can attack your enamel and soften it. Your saliva rinses acids away and helps your enamel to re-harden. If you brush your teeth before the enamel has time to re-harden, it can damage the enamel. Waiting a half hour to an hour after eating before brushing may lower the risk of harming your enamel.
When you sip on acidic drinks, the acid washes over your teeth and weakens your enamel. If you sip these drinks several times a day, your teeth are under constant threat from the acid and don’t have a chance to stay strong and protect against decay-causing bacteria. Many popular beverages are highly acidic and may cause tooth erosion.
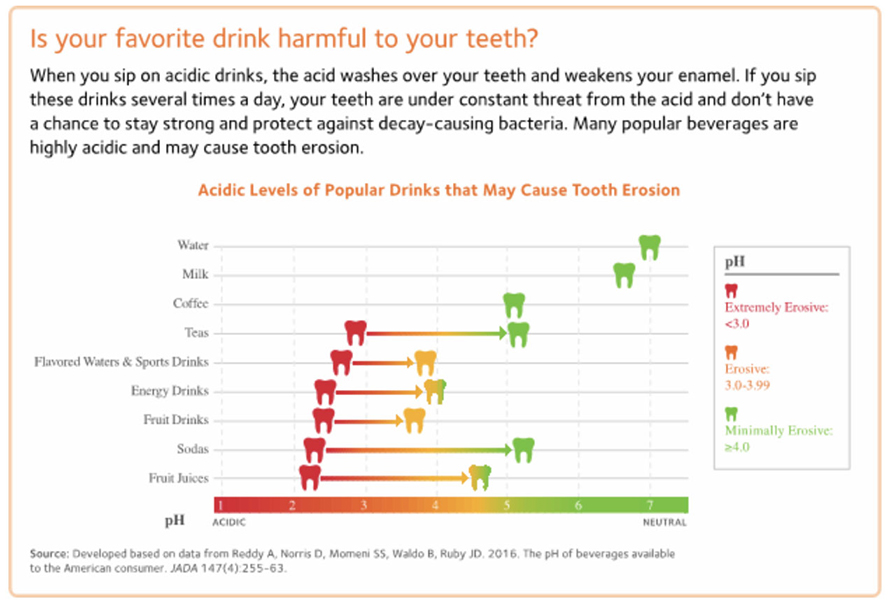
These are some of the common problems that are linked with tooth erosion:
Once the enamel on your teeth wears away, it doesn’t grow back. But, there are ways to manage erosion that can also help to prevent future erosion from happening. What to do about your tooth erosion will depend on what is causing it to happen as well as your own personal health history.
Ways to manage the effects of tooth erosion can include:
A cavity is a hole in your tooth that forms from tooth decay.
When you eat and drink, bacteria in your mouth feeds on the sugars that are found in these foods and drinks. The bacteria create acids that break down the hard, outer layer of your tooth, called enamel (ee-NAM-ul).
You can get a cavity on any tooth and in any place on your tooth. Only a licensed dental professional can treat and repair your tooth once a cavity has formed.

Chewing surface decay
Decay in between teeth

Decay at the gum line

Root decay
When tooth decay gets through your enamel, a cavity can form. Once the cavity forms in your enamel, it can continue to spread deeper into the layers of your tooth.
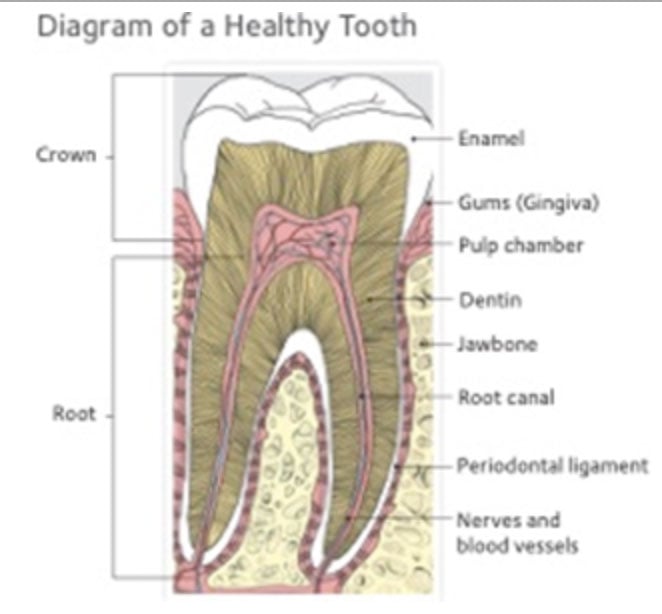
If the cavity gets to the pulp — or center — of your tooth, bacteria from your mouth can infect the nerves in your tooth. This can be very painful. An abscess (AB-sess) — or a pus-filled sac — can form and even become a serious, life-threatening infection if it is not treated.
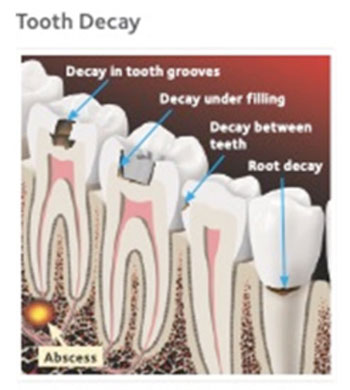
You can have decay on any tooth and in any place on your tooth. It is important to visit your dentist regularly so that any decay can be detected and treated early before it becomes a serious problem, like an abscess or an infection.
What needs to be done to treat your cavity will depend on how far inside your tooth the decay has spread.
Cavities will require some type of filling. This means that the dentist will fill the hole in your tooth with a material that will restore your tooth and protect it from any more damage.
These are a few of the types of fillings your dentist may use to fill your tooth:
Sometimes there is an important reason why one type of filling should be used. You and your dentist should talk about the type of filling that should be used for your tooth.
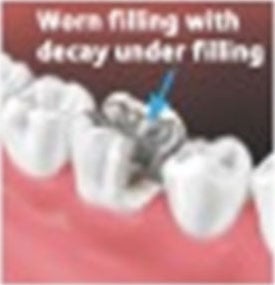

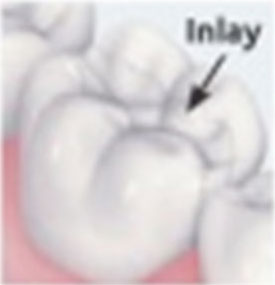
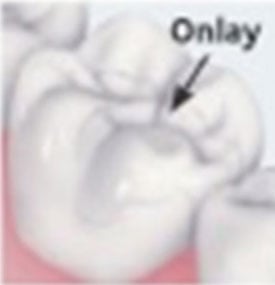
Look for the American Dental Association’s Seal of Acceptance when you are choosing oral care products. These have been scientifically proven to be both safe and effective in fighting cavities and improving your oral health.
Antibiotic prophylaxis (pro-fuh-LAX-is) is when patients take antibiotics before dental treatment to prevent infection. This step is recommended for very few patients.
In the past, anyone who had an orthopedic implant like a hip or knee replacement, or metal plates or rods, used to take preventive antibiotics before certain dental treatments. This is no longer recommended in most cases.
Also, a small number of people with specific heart conditions might be prescribed antibiotics before some dental treatments to help prevent a serious heart infection.
This brochure explains both the possible harms and benefits of taking antibiotics before dental treatment. Use it to help talk with your dentist, physician, orthopedic surgeon or cardiologist to understand whether taking preventive antibiotics is right for you.
People who take antibiotics before some dental treatments usually do so because research suggests that antibiotics may help prevent certain types of infections.
Many people think that there are no harms associated with taking an antibiotic. But, as with any treatment, there are both benefits and potential harms. Because infections after dental treatment are not common and taking antibiotics as a preventative measure may cause a problem rather than defend against one, they are not recommended for everyone.
Here are some problems that can happen with taking preventive antibiotics:
Also, there is scientific evidence that most dental treatment procedures are not connected with prosthetic joint implant infections.
Some people with certain health conditions are told to take antibiotics before having certain dental treatments.
For a small group of people, there’s concern that bacteria in their bloodstream can cause an infection of their heart lining or valves. This infection is called infective endocarditis (end-oh-car-DYE-tis).
The American Heart Association only recommends preventive antibiotics for people who would be at risk of more serious disease if they developed a heart infection after dental treatment. This affects a very small group of people with specific types of heart conditions.
If you have one of these heart conditions, your dentist, physician or cardiologist may recommend that you take an antibiotic before certain dental treatments:
You may be prescribed antibiotics before certain dental procedures to prevent joint implant infections if you
have experienced previous complications from a joint replacement surgery. Or, a person with a total joint replacement might take antibiotics if they are at increased risk of infection because of other drugs or diseases.
Talk to your dentist or orthopedic surgeon before any appointment. They can best determine
if you might benefit from taking antibiotics before your planned treatment.
Antibiotics should always be prescribed by a health care provider and used as directed. If you have any questions, or if there are any changes in your health history or the medicines you take, let your dental office know so they can update your records.
Knowing how to handle a dental emergency can mean the difference between saving or losing your tooth. Here are some helpful tips:
When it comes to protecting your smile during active sports, a properly fitted mouthguard is a key piece of athletic gear. Mouthguards cushion impact that may otherwise cause broken teeth, jaw injuries, or cuts to your lips, tongue or face.
Mouthguards are most commonly used (and may be required) in some contact sports, such as boxing, football, hockey and lacrosse. However, there is evidence that even in other contact and non-contact sports like soccer, baseball, softball, gymnastics or skateboarding, mouthguards help prevent mouth and jaw injuries.
Pick a mouthguard that:
Your dentist can make you or your child a custom mouthguard that is comfortable and protects the jaw. Ready-made mouthguards may be cheaper, but do not fit as well and can make it harder to speak or breathe. The less comfortable the mouthguard, the less likely it will be worn regularly. If it doesn’t fit properly, it is not protective.
If you do choose to buy a ready-made mouthguard, be sure to look for the ADA Seal of Acceptance. Mouthguards that have earned the ADA Seal mean that they were tested and proven to help protect your teeth and mouth from injury when used as directed.
Treating a sports-related dental injury can cost thousands of dollars, so buying a mouthguard can be money well spent. Talk about types of mouthguards with your dentist and select one that works for your needs and budget.
Remember: The best mouthguard is one that fits properly and is worn regularly
The American Dental Association and the Academy for Sports Dentistry recommend that you wear a properly fitted mouthguard if you participate in any of the following activities:
Baseball
Basketball
Bicycling
Boxing
Equestrian Events
Extreme Sports
Field Hockey
Football
Gymnastics
Handball
Ice Hockey
Inline Skating
Lacrosse
Martial Arts
Racquetball
Rugby
Skateboarding
Skiing
Skydiving
Soccer
Softball
Squash
Surfing
Tennis
Track & Field Events
Ultimate Frisbee
Volleyball
Water Polo
Weightlifting
Wrestling
A dental sealant is a thin covering that is applied onto the chewing surfaces of the back teeth. It acts as a barrier to “seal out” plaque and food. Sealants are a safe, painless and easy way to help protect your teeth and keep them healthy.
Sealants on permanent molars reduce the risk of cavities by 80%.
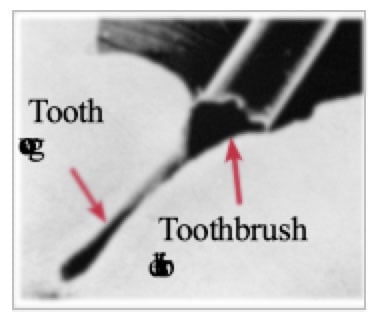 Your teeth are coated with a sticky film of bacteria called plaque (pronounced PLACK). Bacteria in plaque turn sugar from what you eat and drink into acids. These acids can break down the hard, outer layer of your teeth, called enamel (e-NAM-uhl). Over time, the acid can weaken your enamel and may cause tooth decay, or form a hole (cavity) in your tooth’s enamel.
Your teeth are coated with a sticky film of bacteria called plaque (pronounced PLACK). Bacteria in plaque turn sugar from what you eat and drink into acids. These acids can break down the hard, outer layer of your teeth, called enamel (e-NAM-uhl). Over time, the acid can weaken your enamel and may cause tooth decay, or form a hole (cavity) in your tooth’s enamel.
Tooth decay often begins on the chewing surfaces of the back teeth. These surfaces have pits and grooves that trap plaque and bits of food. Toothbrush bristles may not always reach into the pits and grooves, and that makes it hard to keep them clean. The sealant material flows into the pits and grooves on those surfaces to stop bacteria and bits of food from getting trapped.
Even a toothbrush bristle is too big to reach inside a groove in the tooth (magnified).
It takes only a few minutes for your dentist to seal each back tooth.
Sealants are usually clear or white and can’t be seen when you smile or talk.
Sealants can last several years before they need to be replaced. Over time, sealants can come off, which means they will not protect the teeth as well. Chewing on ice or hard foods can also break down sealants. During regular dental visits, your dentist will check the sealants and reapply them if needed.
Sealants are most often placed in children and teenagers. But, you never outgrow the risk of tooth decay and cavities, so adults can benefit from sealants, too.
Sealants are very useful in reducing the risk of tooth decay on the back teeth and may help save you money over time.
When your teeth are healthy, your gum tissue tightly hugs each of your teeth. But, when the gum tissue that surrounds the teeth wears away, or pulls back, exposing more of the tooth or the tooth’s root, it is called gum recession (re-SESH-un), or receding gums. Gum recession can happen at any age and can cause problems for your dental health.
Even if you take good care of your teeth, gum recession is possible. Your dentist can help you understand what is causing your gums to recede and suggest a treatment.
Gum recession can leave the tooth root exposed, or unprotected. The root surface does not have a hard, protective covering like the top of your tooth so it may become sensitive to hot and cold. The exposed tooth root is also more at risk for decay. In severe cases, it may lead to tooth loss.
The risk of gum recession also increases with age.
It is important to treat gum recession so that it doesn’t get worse and cause other problems. The treatment for gum recession depends on the cause.
If gum recession is caused by brushing too hard, your dentist or hygienist can show you a better way to clean your teeth. This will not repair the existing damage, but it will prevent new damage to your gums.
If gum recession is caused by gum disease, the first step is usually a deep cleaning treatment called scaling (SKAY-ling) and root planing (PLAY-ning). Your dentist removes plaque and tartar from your tooth and root surfaces. This helps gum tissues heal and reattach to the tooth. For many patients, this, plus excellent oral care at home and regular dental visits can help control gum disease and recession.
If gum recession is caused by partial dentures that do not fit right, your dentist can adjust or remake them for you.
If your gum recession is advanced, a gum graft may be needed. A thin piece of gum tissue is taken from another place in your mouth and attached where the gum tissue has receded. Once the graft heals, it covers the exposed tooth root and protects it from sensitivity and decay.
Gum grafts are a type of surgery that may be done around one or more teeth. Right after graft surgery, the area may be tender or sore and may swell. Most people are able to go back to their normal routines the next day. However, you may need to avoid chewing for a week or two where the surgery was done. Your dentist will talk with you about your specific healing time.
Diabetes can affect your teeth, gums and the overall health of your mouth.
This brochure reviews the oral health problems that are related to diabetes and the steps you can take to lower your risks and stay on top of your overall health.
Oral Health Problems Related to Diabetes Are:
Gum disease (also called periodontal disease) is when the tissues that hold your teeth in place become irritated and inflamed. If the disease is severe, it can destroy tissue and bone. This can lead to tooth loss. Gum disease is often more frequent and more severe in older adults with diabetes, especially if they smoke.
People with diabetes who have poor blood sugar control are more likely to lose teeth than those who have good control. Research says that treating gum disease may help improve blood sugar control. To help prevent gum disease, eat a well-balanced diet, practice good oral care at home and see your dentist regularly for checkups.
People with gum disease may not see any symptoms. See your dentist immediately if you notice:
Thrush is a fungal infection that happens more often in people with diabetes. It is also more common for people who wear dentures. Possible signs and symptoms include:
Good oral health habits, like brushing and cleaning between your teeth daily, can help you avoid problems with thrush. If needed, your dentist can prescribe medicine to treat it.
If you have diabetes, it may take your body longer to heal after dental work. This includes having a tooth pulled or any other oral surgery. It is important to maintain your blood sugar level to help the injury heal as quickly as possible. Be sure your dentist knows that you have diabetes when planning your treatment.
People with diabetes can be more prone to gum disease. But, if you are careful about keeping your teeth clean, you are less likely to have tooth decay, gum disease and other oral infections. Brush twice a day with fluoride toothpaste for at least two minutes each time. This will remove the sticky film of bacteria on teeth that can lead to gum disease. Also, clean once a day between your teeth with floss or another between-the-teeth cleaner.
Choose toothpaste, a toothbrush and other oral care products that show the American Dental Association’s Seal of Acceptance. This means that the product has met ADA standards for safety and effectiveness.
Your dentist may suggest using a special mouthrinse or toothpaste to control gum inflammation. He or she also may recommend rinsing with a fluoride mouthrinse or applying fluoride at home or in the dental office to help prevent tooth decay.
Getting regular dental exams, professional teeth cleanings and gum disease screenings is important. They can help your dentist spot and treat dental problems early and can help manage the effects of diabetes on your oral health.
If you lost some or all of your natural teeth, dentures can replace your missing teeth. Dentures can be made to look like your natural teeth and can make eating and speaking easier. They can also support your cheeks and lips so facial muscles don’t sag.
There are several types of dentures available and different things to consider for each. This brochure covers three denture options.
Conventional complete dentures have replacement teeth fitted into a plastic base. The base is made to closely match the color of your gums. Any natural teeth you may have will need to be removed before your dentures are placed.
Implant-supported complete dentures are attached to dental implants. Implant-supported dentures require that all your natural teeth be removed. If teeth are removed, your mouth will need to heal before this type of denture can be placed, which could take several months. In some cases, your dentist can make an immediate denture (see below) for you to wear during this healing period.
Not everyone should get implants. This type of denture requires surgery, so you must be in good health and have enough bone to support the implants. Ask your dentist if you are a good candidate for dental implants.
Immediate dentures may be an option for some people. These dentures are made before the remaining teeth are removed. Once the denture has been made, your dentist removes your teeth, and the immediate denture is placed right away.

Conventional complete dentures

Implant dentures

Implants placed in the jaw

Denture fitted over implants
When you get new dentures, your dentist may tell you to wear them most of the time. Dentures should not be worn 24 hours a day, unless recommended by your dentist during the adjustment period. Your dentist may tell you to take them out when you go to bed and put them back in when you wake up.
Wearing your denture around the clock can cause the tissues in your mouth to become irritated.
Your dentist may tell you to use a denture adhesive as you get used to wearing your denture. But, a denture that fits correctly usually only needs saliva to create a tight seal that holds it in place.
Denture adhesive can help a loose-fitting denture for a short time, but if you need to use adhesive all the time, it may be because your denture doesn’t fit correctly. A denture that does not fit well may cause irritation and can lead to mouth sores and bone loss. If your denture is loose, have your dentist check it. If you are using an adhesive, make sure you follow the instructions for use.
Even if you wear dentures, it’s important to take good care of your mouth.
Brush your gums, tongue and the roof of your mouth twice each day with a soft-bristled brush before you put in your denture. Eating a balanced diet is also important to keep your mouth healthy.
You will still need regular oral exams by your dentist even after you have lost your natural teeth. During a visit, your dentist will look for signs of disease such as fungal infection (also called thrush), oral cancer or cancer of the head and neck. Your dentist will also check to see if your dentures fit well or need adjustments.
Like natural teeth, you must take good care of your denture. Plaque and stains can still form on dentures. Here are some tips on how to care for your denture:
Clean your denture every day. Take it out of your mouth and rinse off food particles. Use a special brush made for cleaning dentures or a toothbrush with soft bristles. Brushes with hard bristles can scratch the surface of the denture. Wet the brush and, if you like, you may use a nonabrasive denture cleanser paste to gently clean all surfaces of the denture. You may also submerge your denture in a solution containing denture cleanser for the recommended time.

Be careful when handling your denture. It is delicate and can break if dropped. When removing, handling or cleaning it, try to stand over a sink covered with a towel or filled with cool water in case it falls. Keep your denture away from children and pets when you are not wearing it.
Your dentist is the only person who should make repairs to your denture. Trying to make your own adjustments can harm your denture and your mouth. Don’t use over-the-counter reline materials or glues on your denture. They may contain harmful chemicals and aren’t a long-term solution for fixing your denture.
The normal lifetime of dentures is about 5 to 10 years, but this can vary widely depending on the patient. Your gumline and dental ridge will continue to change in shape and shrink, even if you wear dentures. Over time, dentures may need relining, rebasing or replacing.
Relining is when your dentist adds new material to the underside of the denture base to fit to your gums.
Rebasing is when a new base is made using your existing denture as a model. The artificial teeth from the old denture are used on the new base.
It’s important to replace worn or ill-fitting dentures before they cause problems. Your mouth changes naturally with age. Your jaws may line up differently as bones and gum ridges recede and shrink. At some point, your dentures might not fit well and may need to be remade. Your dentist will let you know when it’s time to replace your dentures.
For more information about taking care of your mouth and teeth, visit MouthHealthy.org, the ADA’s website just for patients.
Produced in cooperation with the American College of Prosthodontists
Periodontal (perry-o-DON-tal) disease is an infection that affects the tissues and bone that support your teeth. It is also called gum disease.
When your gums are healthy, your gum tissues tightly hug each of your teeth. When you have gum disease, your gums pull away from your teeth and may become red, puffy and swollen. As the gum disease gets worse, the tissues and bones that support your teeth can become damaged.
Over time, your teeth may need to be removed. Treating gum disease in the early stages is very important and can help prevent tooth loss.
You may notice one or some of these warning signs, or you may not have any signs of gum disease at all. This is why it’s important to see your dentist regularly — treatment of gum disease is most successful when it’s caught early.
Plaque is a sticky film that is always on your teeth. Bacteria that live in the plaque can make your gums red, puffy and swollen. When plaque is left on your teeth and gums, it can harden. Hardened plaque is also called tartar (TAR-ter). Tartar on your teeth makes it hard for you to keep your teeth and gums clean on your own.
Gums that are red, puffy and swollen also may start to pull away from your teeth. Spaces called pockets start to form between your gums and teeth. These pockets give bacteria a place to collect and grow. The bacteria in your pockets will cause your gum disease to get worse.
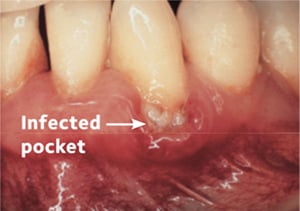
Pockets between your teeth and gums collect bacteria, which can cause them to get infected and inflamed.
Your teeth are held in place by gums, bone and connective tissues (like ligaments). Your gums hug your teeth tightly and there is little or no buildup of plaque and tartar on them.
The bacteria in plaque make your gums red, tender and swollen. Your gums might bleed at this stage. You can also have gingivitis and not have any signs of it. Gum disease at this stage is usually reversible with a professional cleaning by a dentist or dental hygienist followed up with your own good daily home care by brushing and cleaning between your teeth.
In time, as plaque and tartar build up where your teeth and gums meet, the gum tissues and bone around your teeth begin to break down. Periodontitis affects about 42% of adults over age 30 in the United States.
Your teeth become loose and may need to be removed by a dentist. This stage is very serious and may require surgical treatment.
When checking for periodontal disease, your dentist or hygienist uses an instrument called a periodontal probe to gently measure the depth of the pockets around each of your teeth. When your teeth are healthy, the pocket depth should be 3 millimeters (mm) or less. Usually, the more severe the disease, the deeper the pocket. This means more advanced loss of bone attachment, allowing the bacteria to have more room to grow and cause serious damage to your gums and bone, loosening your teeth.

Periodontal probe of healthy gums.
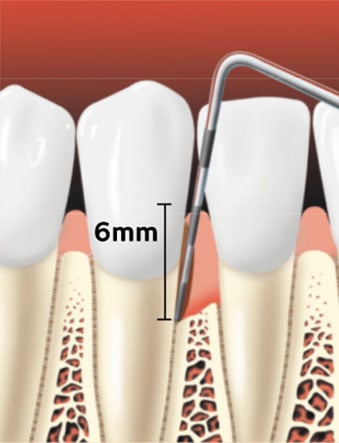
Periodontal probe showing a pocket forming between the tooth root and the gums.
Dental x-rays can check for the amount of bone supporting your teeth. If low bone levels are spotted, it could be a sign of damage from gum disease.

Healthy gums have bone that supports the teeth.
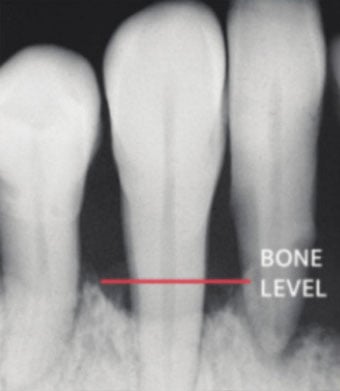
Gum disease can create bone loss.
Anyone can get periodontal disease. There are a few factors that can increase your risk of getting periodontal disease:
Gum disease may also be seen more often in people with diabetes or those with some forms of heart disease.
It’s important to talk to your dentist about medications you may be taking or health problems you may have. Together, you can work out an oral care plan for your best oral health.
Your treatment will depend on factors such as your personal health history and the stage of your gum disease.
Your dentist may also refer you to a periodontist — a dentist who specializes in the treatment of gum disease. A periodontist is well versed in the surgical treatment of gum disease.
If the gum disease is caught early enough (while it is still gingivitis), you may simply need a professional cleaning and improved home hygiene. Your dental team can also give you advice for improving your daily oral hygiene.
A professional cleaning is not enough if your gum disease is severe. Usually a special deep cleaning called scaling (SKAY-ling) and root planing (PLAY-ning) is needed.
During scaling, your dentist or hygienist carefully removes plaque and tartar down to the bottom of each periodontal pocket.
The next step is root planing, which is cleaning and smoothing your tooth’s root surfaces. Smoothing the surfaces helps your gums heal and reattach to the tooth, shrinking the pocket depth.
Scaling and root planing may take more than one visit depending on the amount of treatment you need.
At follow-up visits, your dentist or hygienist will measure the pocket depths to see if scaling and root planing has been successful. If the pockets have deepened and the supporting bone is lost, more treatment may be necessary.

Scaling removes plaque and tartar from below the gumline.

Root planing smothes the tooth root and helps the gums reattach to the tooth.

Healed pocket after treatment.
If the pockets do not heal enough after scaling and root planing, periodontal surgery may
be needed. Surgery allows your periodontist or dentist to remove tartar and plaque from hard-to-reach areas.
After surgery, your gums are stitched into place to tightly hug your teeth. Surgery can reduce pocket depth and make it easier to keep your teeth clean.
If bone has been damaged by gum disease, you may need surgery to rebuild or reshape the bone.
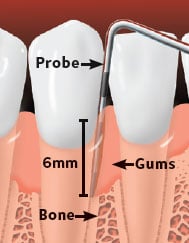
Probe shows pockets due to gum disease. Gums are inflamed and bone loss has occured.

The bone is reshaped and any remaining tartar is removed.

Healed site after periodontal surgery.
You don’t have to lose teeth to periodontal disease. Brush, clean between your teeth, eat a healthy diet and schedule regular dental visits for a lifetime of healthy smiles.
It generally costs much less to keep your teeth and gums healthy than to wait until you have a problem that needs to be treated.
This owner’s manual will cover what you need to know so you can keep your mouth healthy and your smile looking great. It will also tell you about the options for treating your teeth and gums if you’ve begun to experience any mouth disease. Keep in mind that your dentist is a key partner in achieving your goal of excellent oral health. He or she can help you decide which dental options are right for you.
This manual explains:
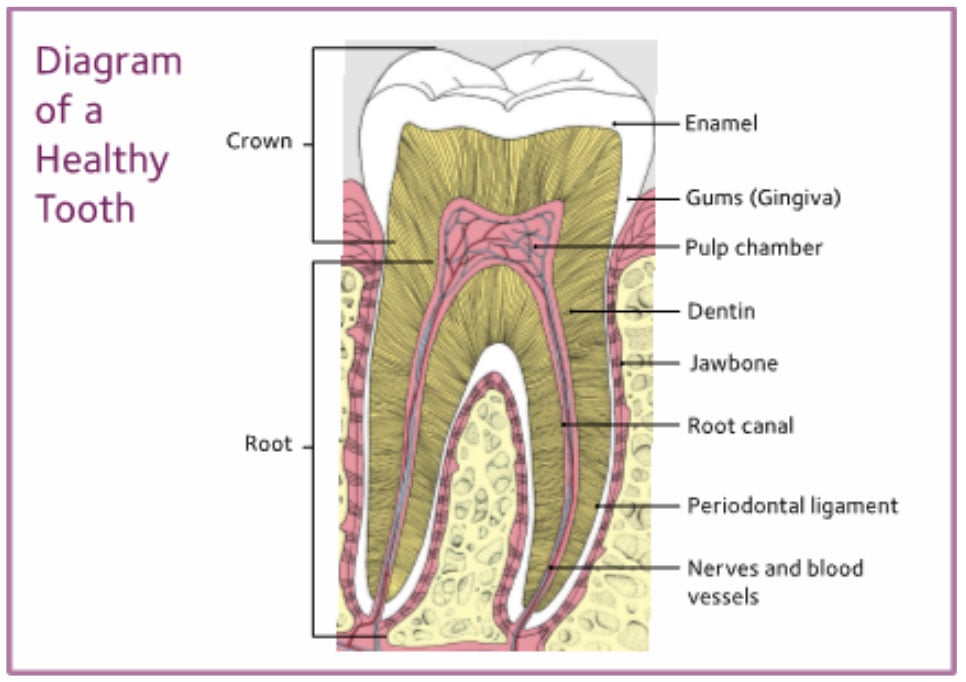
Your tooth looks like one solid piece, but it has many layers. Take a look at the picture of the inside of the tooth on page 2. You’ll see that there are two main parts of the tooth: the crown and the root.
The crown is the part of the tooth you can see. It includes:
The part of the tooth you can’t see is the root; it holds the tooth in place in your jawbone. Your tooth’s roots need to be healthy so they stay strong and can keep your teeth in the right position. This helps your teeth work together so you can eat and speak properly — and makes your smile look great, too!
The root part includes:
Taking good care of your teeth and gums isn’t just about preventing cavities or bad breath. Your mouth is a window into the health of your body. It can show if you are not eating foods that are best for you or signal that you may be at risk for a disease. Diseases that lower your body’s ability to fight infections may raise your risk of oral diseases. Gum disease may also be connected with other health issues, such as type II diabetes, some types of heart disease and stroke. However, a link between these conditions and gum disease does not mean that one condition causes the other.
It’s important to keep your teeth and gums healthy to prevent tooth decay and periodontal (perry-oh-DON-tal) disease, also known as gum disease. This is especially true because gum disease and other health problems may be linked.
Here are the basic steps to keeping your mouth healthy:
Daily cleanings are important to prevent tooth decay and periodontal disease. This is because your teeth are covered with a sticky film of bacteria called plaque. Plaque that is not removed can irritate your gums, making them swollen or causing them to bleed. This is called gingivitis (jin-ji-VY-tis), the early stage of periodontal disease.
Brushing and cleaning between your teeth every day helps remove food particles and plaque from your mouth. Here are some tips on making good oral care part of your daily routine:
Your dentist or hygienist can show you how to properly brush your teeth. Here are some tips to get you started:

Place your toothbrush against your gums at a 45-degree angle. Move the brush back and forth gently and in short strokes, about as wide as each of your teeth.

Brush the outer tooth surfaces, keeping the toothbrush at an angle to the gums.

Brush the inner tooth surfaces.
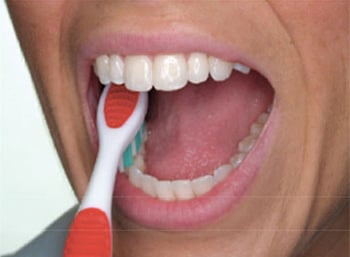
Brush the chewing surfaces.

Use the top part of the brush to clean the inside surface of the top and bottom front teeth. Use a gentle up-and-down motion.


When shopping for oral health care products like toothbrushes, between-the-teeth cleaners or mouthrinses, look for the ADA Seal of Acceptance on the package. The Seal tells you that the product has met the ADA’s standards for safety and effectiveness.
Flossing might feel clumsy at first. It takes a little time to get the hang of it. Here are some tips on how to floss:
1. Break off about 18 inches of floss and wind most of it around one of your middle fingers. Wind the remaining floss around a finger on the other hand. This finger will take up the used floss.
2. Hold the floss tightly between your thumbs and forefingers. Guide the floss between your teeth, using a gentle rubbing motion. To avoid injuring your gums, never snap the floss into gum tissue.

3. When the floss reaches the gumline, curve it into a “C” shape against one tooth. Gently slide it into the space between the gum and the tooth.

4. Hold the floss tightly against the tooth. Gently rub the side of the tooth, moving the floss away from the gum with up and down motions.

5. Repeat this method on the rest of your teeth. As you move from tooth to tooth, unwind the clean floss with one finger and take up the used floss with a finger on the other hand. Do not forget the back side of the last tooth.
You may think that your teeth are in fine shape because you brush and clean between them every day. But, your home care routine is only part of the plan — your dental team plays a very important role, too.
Your dentist can:
Each time you visit the dentist, tell him or her about changes in your overall health, especially if you have been sick lately or if you have any ongoing conditions. Also tell your dentist about all medications, drugs and vitamins you are taking.
If you use tobacco in any form, you are setting yourself up for trouble. Whether you smoke, dip or chew, consider these tobacco-related threats to your oral health:
Many people are turning to electronic cigarettes and vaping devices because they believe they are a safer and possibly healthier alternative to traditional tobacco products like cigarettes, pipes and cigars. However, there is no current evidence that shows e-cigarettes and vaping devices are any safer than regular tobacco products.
Many toxic ingredients are found in both cigarettes and e-cigarettes. It is not easy to quit using tobacco, but it is important. Try to do it the right way and not replace one bad habit with another. Talk to your dentist about ways you can stay motivated to quit.
Tips to help you kick the habit are also online at www.smokefree.gov, or by calling 1.800.QUITNOW.
A well-balanced diet helps you have good energy levels and a healthy weight and can lower the number of times you get sick. It may also improve your chances of avoiding diseases like heart disease, type II diabetes and oral diseases, like tooth decay.
However, certain eating patterns and food and drink choices can lead to tooth erosion and cavities. A steady supply of sugary or acidic foods and drinks, including sports drinks, sodas and energy drinks, can damage your teeth.
Plaque is the sticky film of bacteria that forms on your teeth. When plaque is left on your teeth, the bacteria in the plaque use the sugar in food and drinks to make acid. This acid attacks your tooth enamel. Eventually, your enamel can break down from these acids and cavities can start to form.
When you have sugary or acidic foods or drinks many times a day, it exposes the enamel of your teeth to acid attacks throughout the day. This raises your risk of getting cavities or wearing away the enamel surface. This wearing away is called tooth erosion.
Making the right food and drink choices can help keep your mouth healthy.
Here are some simple steps you can follow:
Gum disease, also called periodontal disease, is very common. It affects people of all ages, and many may not even know they have it.
Gum disease is an infection that affects the tissues and bone that support your teeth.
Healthy gum tissue tightly hugs each of your teeth. When you have gum disease, your gums pull away from your teeth and become red, puffy and swollen. As the disease gets worse, the tissue and bone that support your teeth are destroyed. Over time, teeth may need to be removed. Treating gum disease in the early stages can help keep tooth loss from happening.
It can be hard to know. You can have gum disease without clear signs of it. That’s why regular dental exams are so important.
If you notice any of these signs, see your dentist:
Gum disease is caused by plaque. If your teeth are not cleaned well, your gums can become irritated, swollen and red.
Swollen and red gums can pull away from your teeth and form spaces called pockets. These pockets provide a space for more bacteria. If the infected pockets are not treated, the disease can get worse and the bone and other tissues that support your teeth can be damaged.
Other things that may increase your risk of gum disease include:
A patient with gum disease usually needs more dental visits than a patient without gum disease. Your dental team may treat the disease with a professional cleaning, a deep cleaning called scaling and root planing or sometimes combining cleanings with medication to treat the infection. You may need extra treatment if your gum disease is too far along and a deep cleaning by itself won’t heal your infection completely.
You can fight gum disease with good oral care, regular dental visits and by saying “no” to tobacco products.
Tooth decay is a disease that damages and breaks down the layers of your teeth. When you eat and drink, bacteria in your mouth feed on the sugars that are found in these foods and drinks. The bacteria create acids that break down the enamel.
When tooth decay gets through your enamel, a cavity can form. Once the cavity forms in your enamel, it can continue to spread deeper into the layers of your tooth.
Only a licensed dental professional can treat and repair your tooth once a cavity has formed.
If the cavity gets to the pulp chamber, bacteria can infect the pulp in your tooth. This can be very painful. An abscess (AB-sess) —or a pus-filled sac — can form and even become a serious, life-threatening infection if it is not treated.
A cavity that isn’t treated can lead to pain and loss of teeth. If you have tooth pain, you might not be able to get through your daily routine. You also may not be able to eat or sleep properly and could miss days of work or school.
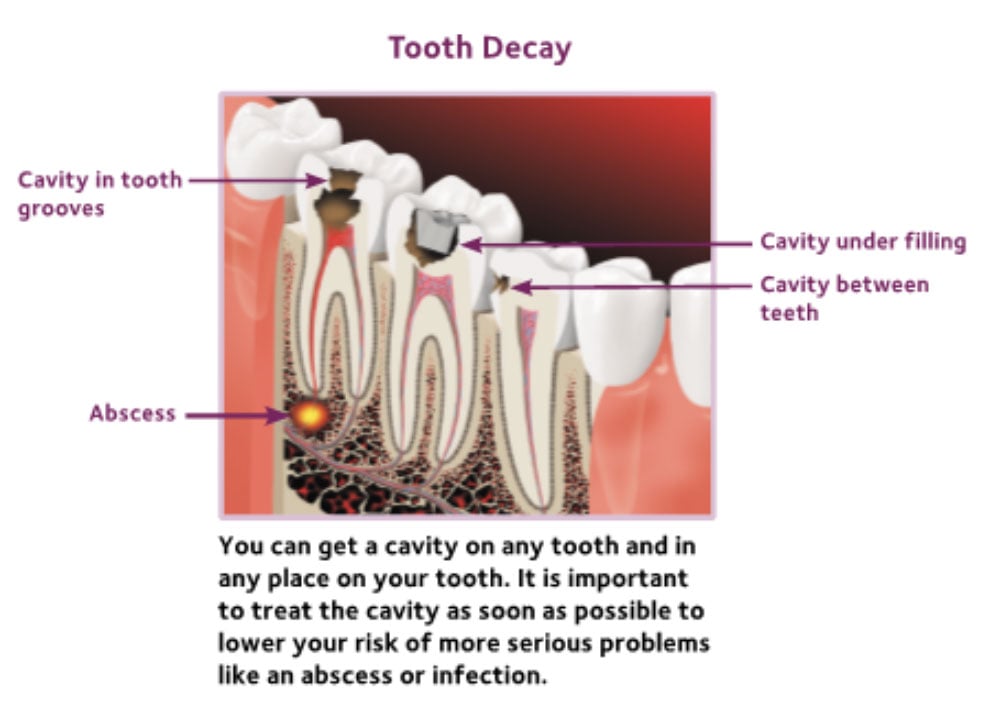
Not exactly, but the bacteria that cause tooth decay can be shared. Bacteria can be passed by kissing, sharing a cup or spoon or anything else that carries a drop of saliva from one mouth to the other. Parents: do not share your toothbrush with your child!
Tooth decay can get worse quickly, but it often takes months for a cavity to develop. Signs of having a cavity can include:
You may notice one or more of these signs. Or, you may not notice any signs at all. The best way to tell if you have a cavity is to visit your dentist for regular appointments.
Treatment for your cavity will depend on how far inside your tooth the decay has spread. Cavities will require some type of filling. This means that the dentist will remove the decay and fill the hole in your tooth with a material that will restore your tooth’s shape and protect it from any more damage.
If your cavity is very large, a filling may not be enough. Your tooth may need to have a crown, an inlay or an onlay placed on it.
If the pulp tissue is infected, you may need a root canal treatment.
If your tooth is badly damaged from a cavity, it may have to be removed. Your dentist will talk with you about your options and the best way to get your mouth healthy again.
It is easier and more affordable to prevent tooth decay than to repair a decayed tooth!
Anyone can experience tooth decay or get a cavity, but here are some steps you can take to help prevent cavities from forming.
By following a healthy oral care routine, making smart food choices and visiting your dentist regularly, you can lower your risk for cavities.
If you are having a dental problem like gum disease or tooth decay, your dentist can recommend a treatment that is right for you. Your dentist can also talk with you about your options for replacing any missing teeth or for otherwise improving your smile.
All of your teeth work together to help you chew, speak and smile. When teeth are missing, it can be difficult to do these things. Also, the loss of a tooth may cause your mouth to sink and your face to look older. If one or more teeth are missing, your dentist can replace them with a dental implant, a fixed or removable bridge or a denture. Discuss replacement options with your dentist to find one that meets your needs. (Also see information on implants on page 18.)
Your dentist has many different techniques to shape and sculpt your smile. With a few simple steps, you can have a smile that will make you feel great. And, treatment may be more affordable than you think.
Here are some issues that can be corrected by dentists:
Many people choose implants to replace a single tooth, several teeth or to support a full set of dentures. Implants are posts that are surgically placed in your upper or lower jaw, where they join with the jawbone and act as a sturdy anchor for replacement teeth.
Dentures, bridges or single teeth mounted to the implants won’t slip or shift in your mouth — a very important benefit when eating and speaking. Implants are also a good value because they can last a lifetime with good care.
However, implants are not an option for everyone. Because implants require surgery, you should be in good general health. Also, you either must have enough bone to support the implant, or be able to grow enough bone. If you smoke or have a chronic illness or high blood pressure, you may not be a good candidate for implants.
Your dentist can help you decide if implant treatment is right for you. There are many different kinds of implants. Treatment can take only one day, or it can take several months, or somewhere in between. Your dentist can outline a treatment plan that is most likely to be successful for you.
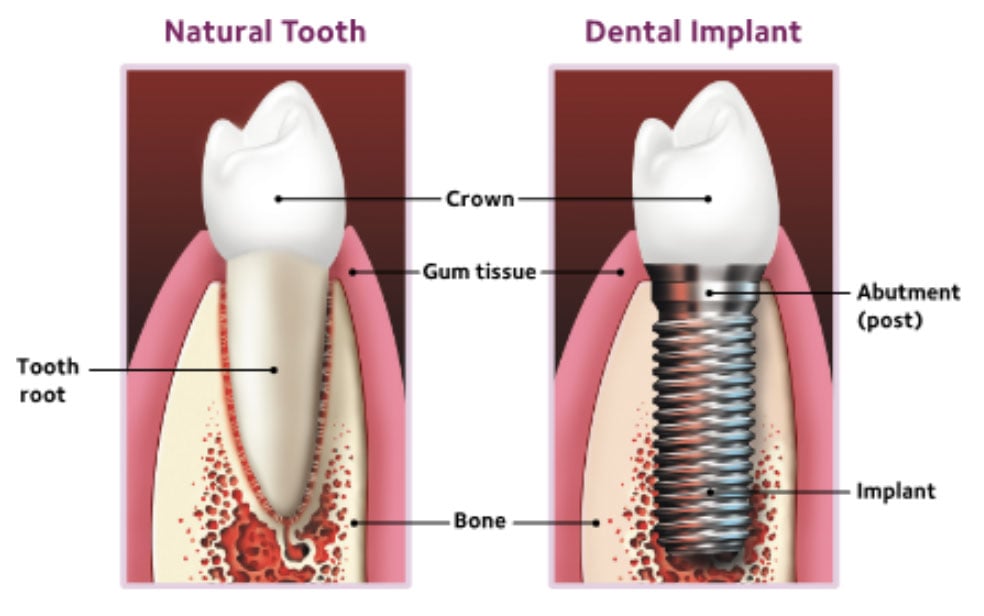
A dental sealant is a thin plastic coating that is put on the chewing surfaces of the back teeth. The sealant material flows into the pits and grooves on those surfaces and acts like a barrier, protecting enamel by “sealing out” bacteria and bits of food that can cause tooth decay.
It is better to prevent tooth decay with sealants than to treat decay after it has already formed. Sealants are very useful in preventing tooth decay on the back teeth and can save you money over time.
Sealants are a safe, painless and easy way to help protect your teeth and keep them healthy. This brochure explains how.
Your teeth are coated with a sticky film of bacteria, called plaque (pronounced PLACK). Bacteria in plaque turn sugar in what you eat and drink into acids. These acids can break down the hard, outer layer of teeth, called enamel (e-NAM-uhl). Over time, acid can weaken enamel and may cause tooth decay, or form a hole (cavity) in your tooth’s enamel.
Tooth decay often begins on the chewing surfaces of the back teeth. These surfaces have pits and grooves where plaque, bacteria and bits of food can get trapped. Just like in the pictures below, toothbrush bristles can’t reach into the pits and grooves, and that makes it hard to keep them clean. Your dentist may recommend dental sealants to keep decay from starting on these chewing surfaces in the pits and grooves.
Nine out of ten cavities children get are on their permanent back teeth. Sealants can prevent most of these cavities by keeping out bits of food and stopping bacteria and acid from settling on teeth.

The chewing surfaces of a molar (magnified) have pits and grooves that trap plaque and bits of food.

Even a toothbrush bristle is too big to reach inside a groove in the tooth (magnified).
Sealants are not a substitute for cleaning your teeth every day! They only help prevent decay if you stick to your daily oral hygiene routine.
Research shows that dental sealants are safe and effective. According to the Centers for Disease Control (CDC), children ages 6 to 11 without sealants have almost three times more cavities than children with sealants.
The American Dental Association (ADA) recommends dental sealants to lower your risk of tooth decay and cavities. If you have any questions, talk to your dentist.
It takes only a few minutes for your dentist to seal each tooth. These are the steps your dentist may use to put sealants on your teeth:
Sealants are smooth and you can’t feel them on your teeth. They are usually clear or white and can’t be seen when you smile or talk.
Sealants usually last several years before they need to be replaced. Over time, sealants can come off, which means they may not protect the teeth as well. Chewing on ice or hard foods can also break down sealants.
During regular dental visits, your dentist will check your sealants and can reapply them if needed.
Sealants are recommended for children and teenagers because tooth decay can start soon after teeth come in. But, you never outgrow the chance of developing tooth decay and cavities, so adults can benefit from sealants, too.
A sealant can be placed on a tooth that does not have a cavity in its pits and grooves. If your tooth is stained or has slight decay, your dentist may suggest you get a sealant, though other treatment may be necessary. If your tooth has more severe decay or has a cavity, it may need a more advanced treatment like a filling.
A message for parents
Regular dental checkups and dental care—such as cleanings, fluoride treatments and sealants—provide your child with “smile insurance.” Plan your child’s first dental visit within 6 months after the first tooth appears, but no later than the first birthday. Consider it a “well-baby checkup” for your child’s teeth.
Many sports-related dental injuries can be prevented by wearing a mouthguard. Mouthguards can be custom-made by your dentist to fit your child’s mouth. Or, you can purchase a “boil-and-bite” mouthguard at sporting goods stores that has the ADA Seal.

The food and drinks you give your child can affect their oral health. Everyone, including your child, has plaque—a sticky film of bacteria that forms on teeth. Plaque can build up if it isn’t removed from your child’s teeth every day. The plaque bacteria feed on the sugar that’s found in the food and drinks you give your child. The bacteria create acids from this sugar supply.
These acids can attack the hard, protective layer of enamel on your child’s teeth for up to 20 minutes after they finish eating and drinking.
Repeated acid attacks can affect your child’s teeth, causing problems like erosion or decay, which can lead to infection in other parts of the body.
For good dental and overall health, be sure your child eats a healthy diet. If your child needs a between-meal snack, choose healthy foods, like fresh fruits, vegetables, and low-fat/high protein foods. To help prevent tooth decay, save sweets for mealtime.
For ideas about healthy foods and drinks to give your child, see www.choosemyplate.gov.

For children under three years old.

For children three to six years old.
Look for the ADA Seal of Acceptance. Choose oral health products that display the American Dental Association Seal of Acceptance. This means they are both safe and effective in keeping your child’s mouth healthy.
Decay in Baby Teeth

Healthy baby teeth

Moderate decay

Moderate to severe decay

Severe decay
Fluoride helps make teeth stronger and protects them from decay. It is a mineral that occurs naturally and is found in many water sources. Children who drink water that has the recommended levels of fluoride are less likely to get cavities than children who do not drink fluoridated water. Fluoride is also found in anti-cavity toothpastes, mouthrinses and treatments applied in the dental office. Talk to your dentist about your child’s fluoride needs. Be sure to tell your child’s dentist if you use well or bottled water; or if you use a water treatment system at home.
A sealant is a plastic material that your dentist can easily apply to the chewing surfaces of your child’s back teeth. The sealant flows into the pits and grooves in the teeth—places where a toothbrush might miss. Sealants protect teeth from plaque and acid attacks.
If your teeth are discolored, tooth whitening may help. “Whitening” is any process that can make teeth look whiter. It may be safely done at home or in a dental office. It is best to talk to your dentist before whitening your teeth.
Tooth-whitening options range from gentle surface whiteners to stronger ones that can also remove deeper stains. There are three main types of tooth whitening products:
Whitening toothpastes help remove stains on the surface of your teeth. They are the gentlest of the whitening options. They work using polishing action rather than chemicals and don’t have many side effects. However, they do not get teeth as white as chemical products. Whitening toothpastes can lighten teeth a little bit
at a time, over days or weeks.
Several whitening toothpastes have earned the American Dental Association’s (ADA’s) Seal of Acceptance and have been shown to whiten teeth by removing surface stains. Look for the Seal when choosing a whitening toothpaste.
Home-use whiteners come from your dentist or are sold over the counter. They may be applied to your teeth using trays, strips, as a rinse, or with a brush. They usually contain a chemical called peroxide (pur-OX-eyed), which gets below the surface to lighten tooth enamel. Home-use whiteners are meant to be used over days or weeks.
Your dentist may make custom whitening trays for your upper and lower teeth. You put the whitening gel in the trays and wear them for short times during the day or overnight. Your dentist will tell you how long to wear them. If you wear the trays for too long, the peroxide in the gel can irritate your teeth.
In-office whitening is done in the dental office. In-office whiteners are much stronger than whitening toothpastes and home-use whiteners because they have more peroxide. They can change the color of your teeth faster than the other methods.
In-office whitening is usually done in about one hour. To help protect your mouth from the peroxide, your gum tissues will be covered with either a thin sheet of rubber or a protective gel. A light or laser may be used in addition to the peroxide.
Tooth whitening is not a good choice for all people. If your gums have pulled away from the teeth in some places, whitening may irritate these areas. If you have tooth decay (cavities) or gum disease, your dentist may recommend that these be treated before whitening. Also, it is important to be aware that the color of fillings, crowns, implants and some stains cannot be changed by tooth whitening.
Talk to your dentist about tooth whitening before you begin. He or she will do an oral exam to find out if it’s right for you.
If you have whitened your teeth recently, they may stain more easily. To keep your teeth white for as long as possible, avoid tobacco products and stain-causing food and drinks (like coffee, tea, and red wine) for several days after whitening. Keep in mind that teeth usually return to their original shade over time. But if you can steer clear of tobacco and large amounts of stain-causing food and drinks, your teeth may stay bright for several years.
Whitening treatment may cause your teeth to be sensitive to very hot or cold temperatures. Whitening may also irritate your gums for a short time. If the side effects do not go away after a few days, see your dentist.
To avoid harming your teeth and gums, always follow the product directions and all instructions from your dentist. If your teeth become very sensitive or if you get sores in your mouth, stop using the products and call your dentist.
There is such a thing as too much whitening! Do not use whitening products for longer than listed in the product directions or by your dentist. Too much whitening can make your teeth and gums hurt badly. It can even harm your tooth enamel.
he complaint of dry mouth — also called xerostomia (zero-STOW-me-uh) — is often caused by a low flow of saliva. Saliva coats and moistens oral tissues. It cleanses your mouth and helps digest foods as they are chewed. But, if you do not make enough saliva, harmful germs can grow in your mouth.
Having a dry mouth all of the time or most of the time can result from other health issues or the treatments for them.
Drying irritates the soft tissues in your mouth, which can make them sore and can lead to infections. Without good saliva flow to keep your mouth clean, tooth decay and oral infections become much more common. Constant dryness may lead to more cavities and bad breath. It can also lead to:
Dry mouth can also make full dentures less comfortable to wear and can cause sores. This is because there is no thin film of saliva to help dentures hold on well to oral tissues.
The most common cause of dry mouth is medications taken to treat other problems. Dry mouth is a side effect of more than 500 prescription and over-the-counter medications. These include medications for:
Read the drug inserts that come with your medications. If you see dry mouth listed as a side effect, tell your dentist, hygienist or physician.
Dry mouth also can be caused by other factors. These can include:
Treatments for dry mouth will depend on the cause. In some cases, a change in medications you are taking may help. Your dentist or physician may suggest that you use a special gel or liquid (available at drugstores) to keep oral tissues moist. Drinking more fluids throughout the day can also help. Other ways to manage dry mouth include:
Regular dental checkups are important if you have dry mouth. Tell your dentist about the medicines you are taking and any health problems you are having.
Without enough saliva, tooth decay can also occur. You must take good care of your teeth and gums to help prevent tooth decay and gum disease. Brush twice a day with a fluoride toothpaste and for two minutes each time. Use floss or use another between-the-teeth cleaner at least once a day. This will remove bits of food from tight places your toothbrush cannot reach.
 When choosing a dental product, check to see if it has the American Dental Association Seal of Acceptance. This means the product is proven to be safe and effective.
When choosing a dental product, check to see if it has the American Dental Association Seal of Acceptance. This means the product is proven to be safe and effective.
Together, you and your dentist can manage dry mouth to bring you relief.
Tooth decay often occurs on the chewing surfaces of back teeth. The good news is that sealants can help protect these surfaces from tooth decay and improve your chances to stay filling-free.
What causes tooth decay? Your teeth are coated with a sticky film of bacteria called plaque (pronounced PLACK). The bacteria convert the sugars you eat and drink into acids that attack the strong, outer layer of your tooth, called enamel. Over time, this can weaken the enamel and cause cavities.
Even a toothbrush bristle is too big to reach inside a groove in the tooth (magnified).
What is a sealant? A sealant is a material applied to the chewing surfaces of your back teeth, which have deep pits and grooves. The material flows into these pits and grooves and then hardens. Once your teeth are sealed, food and plaque cannot get in. The sealant forms a barrier against acid attacks.
How are sealants applied? Your teeth are cleaned and the chewing surfaces are prepared to help the sealant stick to your teeth. The sealant is painted onto the chewing surface where it bonds to your tooth and hardens. Sometimes a special light is used to help the sealant harden. It usually takes only a few minutes to seal each tooth.
How long do sealants last? Sealants may last several years and can be reapplied if needed. As long as the sealant stays undamaged, the tooth surface will be protected from decay (cavities). During your regular dental visits, your dentist will check the sealants and reapply them if needed.
How else can I protect teeth from decay? Sealants protect only the chewing surfaces of teeth. Good care of your teeth at home along with regular exams and cleanings at your dentist’s office are just as important. These good habits reduce your chance of cavities in all of your teeth. Be sure to:
Having dental coverage can make it easier to get the dental care you need. But, it’s important to understand that most dental benefit plans do not cover all dental procedures. When deciding on your treatment, dental benefits should not be the only thing you consider.
You should know what your dental plan covers and what it doesn’t. This brochure can help you understand why your dental benefit plan may not pay for all or even a portion of your recommended treatment. Ultimately, your treatment should be determined by you and your dentist — not by your level of dental coverage.
Dental benefit plans are not designed to cover all dental procedures. Plans usually cover some, but not all, of your dental costs and needs.
Many plans involve a contract between your employer and a dental plan provider, but you can also buy individual plans on your own or through the Health Insurance Marketplaces.
Your dentist’s primary goal is to help you maintain good dental health, but not every procedure your dentist recommends will be covered. To avoid surprises on your bill, it’s important to understand what and how much your plan will pay.
Your employer and the plan provider agree on the amount your plan pays and what procedures are covered. Your dentist is not involved in deciding your level of coverage.
Your dental coverage is not based on what you need or what your dentist recommends. It’s based on how much your employer pays into the plan. Sometimes, you may have a dental care need that is not covered by your plan. Employers generally choose to cover some, but not all, of employees’ dental costs.
There are certain cost-control measures that dental benefit plans use to determine how they share treatment costs with you.
Here are some key terms that are used to describe these measures:
A deductible is the amount of money that you must pay before your benefit plan will pay for any service. It can take more than one service or visit to meet your deductible. Most plans don’t require a deductible for preventive services like cleanings and exams or for diagnostic services.
In most cases, after you meet your deductible you will be expected to pay a percentage of the allowed benefit amount of a covered dental service. This is called coinsurance.
For example: Your plan may pay 80% and you pay the remaining 20% owed to your dentist. If your bill was $100, then your plan pays $80 and you would pay the remaining $20.
This is the maximum dollar amount a dental plan will pay during the year. Your employer decides the maximum levels of payment in its contract with the dental benefit provider. You would pay for anything over that set dollar amount.
For example:
Your dental expenses: $3,500
Your annual maximum: $2,000
You owe: $1,500
If the annual maximum of your plan is too low to meet your specific needs, you may want to ask your employer to consider a higher annual maximum. If your plan also covers braces, there is usually a separate lifetime maximum limit.
Your dental plan may not cover conditions you had before enrolling even though treatment may still be necessary. You would be responsible for paying these costs.
For example: If you had a missing tooth before the effective date of your coverage, then benefits will not be paid for replacing the tooth. Even though your plan may not cover certain conditions, you may still need treatment to keep your mouth healthy.
These terms apply to patients covered by more than one dental plan. The benefit payments from all plans should not add up to more than the total charges. Even though you may have two or more dental benefit plans, there is no guarantee that all of the plans will pay for your services. Sometimes, none of the plans will pay for the services you need. Each dental plan handles COB in its own way. Please check your plans for details.
A dental plan may limit the number of times it will pay for a certain treatment. But, you may need a treatment more often to maintain good oral health. Make treatment decisions based on what’s best for your health, not just what is covered by your plan.
For example: Your plan might pay for teeth cleaning only twice a year, but you need a teeth cleaning 4 times a year, so you would pay out of pocket for the extra 2 cleanings.
Many dental plans state that only procedures that are medically or dentally necessary will be covered. If the claim is denied, it does not mean that the services were not necessary. Treatment decisions should be made by you and your dentist.
If your plan rejects a claim because a service was “not dentally necessary,” you can appeal. Work with your benefits manager and the plan’s customer service department or your dental office to appeal the decision in writing.
For example, your dentist may recommend an implant for you, but the plan may only cover less costly dentures. You should talk with your dentist about the best treatment option for you.
Although you may be tempted to make decisions about your dental care based on what your dental plan will pay, remember that your health is the most important thing. Talk with your dentist to make sure you are getting the treatment that will get your mouth healthy again.
If you have periodontal (perry-o-DON-tal) disease (also called gum disease), you may already have had a special deep cleaning called scaling and root planing. You also may have had periodontal surgery. The periodic cleanings recommended after these treatments are called periodontal maintenance therapy.
The purpose of these cleanings is to help you keep your gums healthy and make sure that periodontal disease does not get worse.
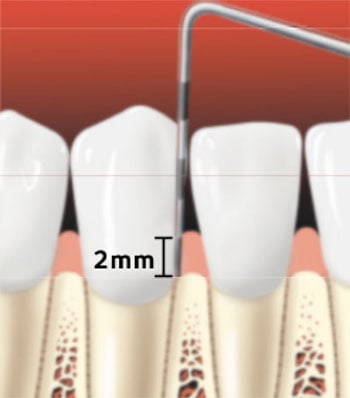
Periodontal probe of healthy gums
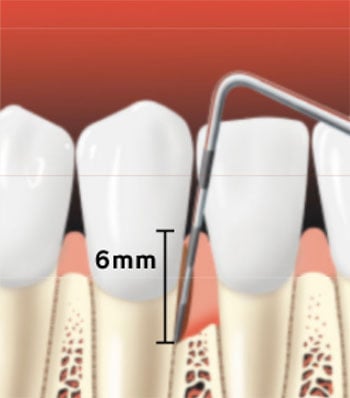
Periodontal probe showing a pocket forming between the tooth root and the gums
Once your periodontal disease is brought under control, it is very important that you get dental care on a regular basis. Cleaning your mouth every day at home is critical, but it’s not enough on its own to keep your gum disease under control. Professional dental care is needed to help control gum disease.
Periodontal maintenance involves a cleaning that goes deeper below the gumline than a regular dental cleaning. You need deeper cleanings because spaces have formed between your teeth and gums. These spaces are called periodontal pockets. Bacteria collects in these pockets and eventually the bone that supports the teeth may be destroyed. The deeper the pocket, the worse your gum disease may be. Periodontal maintenance helps to keep pockets from getting deeper, allowing your gums to heal.
If the bacteria continue to grow, your gums can become red, puffy, swollen and no longer tightly hug your teeth. This can also create bone loss, which causes your teeth to become loose.
With periodic maintenance, the amount of plaque bacteria is lowered. Then, the inflammation can get better, pockets can shrink and your gums can become healthier.
Once gums are healthy, periodic cleanings can help keep them free from infection. Your dentist may also recommend and use medicines to help lower the periodontal bacteria in your mouth. The medicine could be a pill, a special mouthrinse or a medication that your dentist places right into the pocket after you have a deep cleaning.
You will need to see your dentist more often than other people. The pockets and other issues from your gum disease will make it harder for you to clean plaque from your teeth on your own. Your dentist will recommend a treatment schedule that is based on your diagnosis. Be sure to keep all dental appointments.
Your dentist may also refer you to a periodontist (perry-o-DON-tist) — a dentist who specializes in the treatment of gum disease. A periodontist is well versed in the surgical treatment of gum disease. Your visits may switch between your dentist and your periodontist.
Periodontal maintenance appointments are more frequent than regular cleanings, sometimes as often as every 3 to 4 months, depending on your condition. Over time, fewer appointments may be necessary. Even if you don’t feel any pain, your gum disease may not have healed completely, so it’s important to keep all your appointments and continue with at-home care. If you follow through with your maintenance, you are more likely to keep your teeth. If not, your gum disease may get worse.
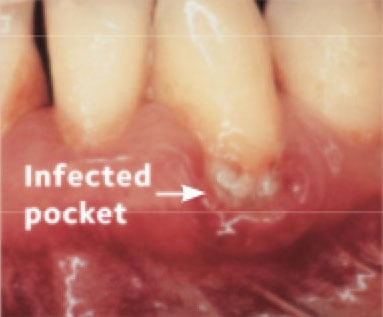
Before Treatment

After treatment
Your teeth and gums may be sensitive after your treatment. This soreness may make
you want to avoid cleaning the treated areas. But it’s important to follow your dentist’s instructions on home care! If plaque is not removed, root decay may form. Talk with your dentist or hygienist to see if a special toothpaste or other treatments can lower your tooth sensitivity.
Brushing and cleaning between your teeth daily are important for everyone, but even more so if you have gum disease. You should brush your teeth two times each day with a toothpaste that contains fluoride.
 Use floss or another between-the-teeth cleaner every day to remove the plaque and bits of food between your teeth and gums. If your gums have pulled away from your teeth, special brushes and wider types of floss and picks may be good choices for you.
Use floss or another between-the-teeth cleaner every day to remove the plaque and bits of food between your teeth and gums. If your gums have pulled away from your teeth, special brushes and wider types of floss and picks may be good choices for you.
Your dentist or hygienist may recommend that you use a mouthrinse or powered toothbrush. Look for the American Dental Association Seal of Acceptance on all dental care products. The ADA Seal tells you that the product meets ADA standards for safety and effectiveness.
Use floss or another between-the-teeth cleaner every day to remove the plaque and bits of food between your teeth and gums.
With the help of your dental team, you don’t have to lose your teeth to gum disease. Periodontal maintenance is most effective if you and your dental team work together.
Your dentist has treated your gum disease, but you must also do your part and take good care of your teeth and gums at home every day.
Check with your dental plan when you are planning treatment with your dental office.
However, you should make treatment decisions based on what’s best for your health, not just what is covered by your plan.
If your treatment is not fully covered by insurance, ask the dental office if it has a payment plan to cover the rest. Keep in mind that having periodontal treatment now may be less expensive than replacing a tooth lost to disease!
Clean between your teeth once a day to help remove food and plaque from under the gum line. Flossing is one way to do this. It takes time to get the hang of flossing. Be patient with yourself and don’t give up!
Your dentist or dental hygienist can show you the right way to floss. Here are some tips that may help:
For a clean, healthy smile, remember to:

What’s the best way to fight tooth decay and gum disease? Pick up that toothbrush twice a day!
Brush your teeth for two minutes twice a day and use a toothpaste with fluoride (FLOOR-eyed), a natural mineral that helps make teeth stronger.
Choose a soft-bristled toothbrush in a size and shape that fits your mouth comfortably. Replace your toothbrush every three months, or sooner if the bristles are worn or frayed. Both manual and powered toothbrushes are effective at removing plaque.
Your dentist or dental hygienist can show you how to brush. Here are some tips to help you start a good routine:

Place your toothbrush against your gums at a 45-degree angle. Move the brush back and forth gently and in short strokes, about as wide as each of your teeth.

Brush the outer tooth surfaces.

Brush the inner tooth surfaces.
Brush the chewing surfaces.

Use the top part of the brush to clean the inside surface of the top and bottom front teeth. Use a gentle up-and-down motion.
Eating a healthy diet, limiting snacks and visiting your dentist regularly will help you keep your smile healthy for years to come.
For a clean, healthy smile, remember to:
IMAGE NEEDED
While you are pregnant, continue to see your dentist regularly for oral exams and teeth cleanings. It is generally safe to have dental treatment during pregnancy.
It’s important for your own health as well as your child’s to have a healthy mouth before your child is born. A wide variety of bacteria live in your mouth, which is normal. When certain types of bacteria outgrow the others, this can lead to gum disease or tooth decay. Pregnancy can make your gums more sensitive to plaque, the sticky film of bacteria on your teeth. Your gums may become red and tender. They may bleed easily when you brush your teeth. This condition is an early stage of gum disease, called gingivitis (jin-ji-VY-tis).
Gingivitis is common in pregnant women, and it can lead to more serious diseases of the gums and bone that hold your teeth in place. Your dentist may recommend that you get your teeth cleaned more often during your pregnancy.
You can lower your risk of developing tooth decay and gum disease by brushing your teeth twice a day and cleaning between your teeth daily.
What you eat during pregnancy affects the growth of your developing baby — including their teeth. Your baby’s teeth begin to develop between months 3 and 6 of pregnancy. So, it’s important that you take in enough nutrients, especially calcium, protein, phosphorous, and vitamins A, C, and D.
Be sure to get enough calcium in your diet for you and your baby by having at least 3 servings of dairy products or other calcium-rich foods each day. Or, your obstetrician (OB/GYN) may recommend that you take calcium pills.
You do not lose calcium from your teeth during pregnancy. Your diet — not your teeth — provides the calcium your baby needs.
Other than water, sugar is in almost everything else that a baby drinks, including breast milk and formula. When teeth are in contact with liquids that contain sugar, decay can start. If decay is not treated, it can destroy baby teeth. That’s why it’s important for you to get in the habit of cleaning your baby’s teeth every day.
As your child gets older, they may start to eat a more varied diet which may contain fruit juice, sports drinks and even soda. It’s important to be aware that these sugary drinks are known to increase your child’s risk to develop tooth decay.
Tooth decay that’s not treated can lead to pain, loss of teeth, and loss of self-confidence. Children with tooth pain can’t eat or sleep properly and may miss days of school. Even worse, decay may lead to an abscess (pus-filled sac) formation, which can cause serious or even life-threatening infections
if it’s not treated.
Tooth decay can be prevented with good oral care. Taking time to prevent tooth decay from starting is less costly than repairing a decayed tooth.
Brushing and flossing remove plaque, the sticky film of bacteria on your teeth. Brush your child’s teeth (and yours!) 2 times a day and for 2 minutes each time. You should clean between teeth with floss or another between-the-teeth cleaner every day.
Brushing teeth the right way is important. You should brush your child’s teeth until they have the skills to do it the right way on their own. If your child cannot tie their own shoes, then they are probably not ready to brush by themselves.
When you teach your child how to brush the right way, it may help to stand behind them and hold the brush while they watch in the mirror. Teach them to spit out all of the toothpaste after brushing.
Even after your child starts to brush their own teeth, you should still watch while they brush. This helps you make sure that they are cleaning their teeth the right way.
By around age 10 or 11, most children should be able to brush their teeth without supervision. If you’re not sure if your child is ready, talk to your dentist or dental hygienist.
Make choosing a toothbrush a fun activity for you and your child. Find a child-sized toothbrush with soft bristles. Let your child pick the color and design. Make getting a new toothbrush a regular treat. You can also ask your dentist or hygienist if there is a powered toothbrush that is right for your child.
For children under 3 years old, use a smear or grain-of-rice sized amount of toothpaste.
For children 3 to 6 years old, use a pea-sized amount of toothpaste.
Place the toothbrush against the tooth where it meets the gums (also called the gum line).
Use a 45 degree angle to make sure you are fully reaching the gum line as well as the tooth surface.
Move the brush back and forth gently in short, soft circles. Brush the outer surface of each tooth. Use the same strokes for the inside surfaces and chewing surfaces of the teeth.
Cleaning between your child’s teeth with floss or a floss aid removes plaque where toothbrush bristles can’t reach.
Begin using floss or a floss aid when your child has 2 teeth that are next to each other. Flossing is not easy for children to do by themselves. The ADA recommends that you floss your child’s teeth daily until they can do it alone, around age 10 or 11.
A. Break off a good amount of floss and wind most of it around your middle or index finger.
B. Wind the rest of the floss around the same finger on your other hand. This finger will take up the used floss.
C. Hold the floss tightly between your thumbs and index fingers.
D. Guide the floss between your child’s teeth, using a gentle rubbing motion. Don’t snap the floss into their gums.
E. Sometimes children as young as 5 years old can use a floss aid.
When your child is ready to floss, show them how to hold the floss so they can gently clean between their teeth. Just like with brushing, it’s a good idea to watch them floss to make sure they are cleaning between all their teeth — including those in the back, which may be harder to reach.
Look for the ADA Seal of Acceptance when choosing products like toothbrushes, toothpastes, floss, and floss aids. The ADA Seal means that the products have been tested and shown to be safe and effective.
Food choices and eating patterns can affect whether your child has problems like tooth decay and cavities. A healthy diet that limits sugary beverages and snacks is good for overall well-being as well as for healthy teeth. A steady supply of sugary foods and drinks, including sports drinks, sodas, and energy drinks, can damage teeth. Acid from sugary foods and drinks can attack teeth for 20 minutes or longer. Over time, tooth decay can happen and cavities can form.
Offer water when your child is thirsty and nutritious foods such as fruit, carrot sticks or cheese if your child is hungry. These are healthier options than giving them cookies, candy, potato chips, and other sweet or sticky foods. Save sweets as an ending for mealtime, when the mouth makes more saliva to help rinse out food particles. Be aware that constant snacking, even snacking on nutritious foods like oranges and dried fruit, can increase risk of cavities because it means teeth are exposed to acid throughout the day.
Avoid giving your child snacks like sodas, chips, cookies, crackers, and candy. All of these can increase your child’s risk of tooth decay and cavities.
For good dental and overall health, be sure your child eats nutritious foods from the major food groups. For more information about a healthy diet, visit choosemyplate.gov.
Fluoride (FLOOR-eyed) is a mineral found in all natural sources of water — even the ocean. Fluoride helps protect tooth enamel from the acid attacks that cause tooth decay. It also helps repair weakened enamel before cavities form.
Children who drink tap water that has the recommended level of fluoride are less likely to get cavities than children who do not drink fluoridated water. If you are not sure your tap water has fluoride, ask your dentist.
Children get added protection from fluoride by getting it from more than one source. Other sources of fluoride include fluoride toothpastes, fluoride mouthrinses, and fluoride treatments applied in the dental office. Talk to your dentist or hygienist about your child’s fluoride needs. Be sure to let them know if you use bottled water or a water treatment system at home.
During a dental visit, your dentist and hygienist will check your child’s mouth for gum and tooth health (no decay!). Tooth alignment and growth patterns will be monitored to watch for problems with your child’s bite. Your dentist will also check to see that all of your child’s teeth are being cleaned properly.
Children’s needs differ, and your dentist is best able to suggest a schedule of visits for your child. The schedule of visits will depend on things like your child’s eating habits, how well their teeth are cleaned, past treatment needs, and water fluoridation in your area.
Baby teeth (also called primary teeth) help your child chew and speak. They also give the face its shape and hold space for adult teeth to come in the right way. These are just some of the reasons why it is so important to take good care of baby teeth!
Baby teeth start to come in when a child is about 6 months old. By age 3, most children have a full set of 20 baby teeth. Spaces between baby teeth are normal. It is also common that some teeth are in contact with those on either side.
Baby teeth fall out as your child develops and grows. This makes room for adult teeth (also called permanent teeth), which begin to come in around age 6.
This chart shows the name of each baby tooth and when each tooth usually comes in (erupts) and falls out (shed). Not all children get the same teeth at the same times. Your child’s teeth may come in earlier or later than shown here.
As teeth come in, babies may have sore or tender gums. To help your baby feel better, you can:
Do not use benzocaine-containing over-the-counter teething products such as Anbesol®, Hurricaine®, Orajel®, and Orabase® and some prescription products to soothe sore gums in young children. These products can cause serious reactions in children. Details are available on the U.S. Food and Drug Administration website: fda.gov.
Pacifiers:
Bottles, Sipping, and Snacking:
Breastfeeding:
Clean your baby’s teeth to prevent cavities
Many infants and young children like to suck on thumbs, fingers, or pacifiers. Sucking is a natural reflex and necessary for feeding. However, sucking habits can cause problems. Their teeth may not grow in straight, and their mouth may not develop correctly.
Thumb sucking and pacifier sucking habits can cause problems as your child’s teeth and mouth develop, like crooked teeth and changes to the shape of their face and mouth.
Children should stop using pacifiers by age 2 and should stop sucking their fingers or thumbs by age 4. If this does not happen on its own, here are a few tips to help them to stop:
Your baby should have their first visit with the dentist after their first tooth appears, but no later than their first birthday. This first visit is a “well-baby checkup” for your child’s teeth. It’s best for your child to have a pleasant first meeting with the dentist. Don’t wait until an emergency comes up to introduce them to the dental office!
At this first visit, your dentist and team will:
Children begin to lose their front teeth around age 5 or 6. Between ages 6 and 12, they will usually have lost all 20 baby teeth. By the time they are 12 to 14 years old, most children have all of their adult teeth except their wisdom teeth.
The first adult tooth usually comes in between ages 6 and 7. Your child will have a mix of baby and adult teeth for a while. The smile might look a little uneven, with some big teeth, some small teeth, and even some missing teeth. Smiles even out once all the adult teeth are in place.
Sometimes a baby tooth is lost before the adult tooth below it is ready to come in. If a baby tooth is lost too early, nearby teeth can shift into the open space. When the adult tooth is ready to come into the space, there may not be enough room. The new tooth may be unable to come in. Or, it may come in crooked or in the wrong place.
If your child loses a tooth early, your dentist may recommend a space maintainer. This is a plastic or metal retainer that holds open the space left by the missing tooth. Your dentist will remove this retainer once the adult tooth begins to appear.
This chart gives the names of adult teeth. It also shows when each tooth usually comes in. Not all children get the same teeth at the same times. Your child’s teeth may come in earlier or later than shown here.
A dental sealant is a plastic material that is put on the chewing surfaces of the back teeth. The sealant material flows into the pits and grooves on those surfaces and acts like a barrier, protecting enamel by “sealing out” bacteria and bits of food.
Sealing a tooth is fast and painless. Sealants can last several years before they need to be reapplied. Ask your dentist if sealants will help your child.
What makes a bad bite bad?
Early treatment may help prevent a bad bite or make it less severe.
A bad bite is when the teeth are crowded, crooked, or out of line, or the jaws don’t meet properly. A bad bite may be noticed as early as 2 years of age, but it is usually seen between the ages of 6 and 12, when the adult teeth are starting to come in.
The dentist checks your child’s bite at every visit, which is another reason why regular dental appointments for children are important. If treatment to correct a child’s bite is needed, your dentist may refer your child to an orthodontist. This is a dentist who specializes in treating bite problems. Treatment to correct a bite usually begins when children are between 8 and 14 years old.
Sport-related dental injuries can be prevented by wearing a mouthguard. Mouthguards help to cushion the damage to your child’s mouth from a blow or heavy hit. Dental injuries such as broken teeth, jaw injuries, or cuts to the lip or tongue are reduced when a mouthguard is used.
Use of a mouthguard is usually thought of for contact sports, like boxing, football, hockey, and lacrosse. However, even in non-contact sports like gymnastics or skateboarding, mouthguard use can help prevent or lower mouth and jaw injuries.
Your dentist can make a custom mouthguard that fits your child’s mouth. Treating a sports-related dental injury can cost thousands of dollars, so a custom-made mouthguard for your child is an excellent investment!
If you choose to buy a ready-made mouthguard, be sure to look for the ADA Seal of Acceptance. Mouthguards that have earned the ADA Seal were tested and found to meet ADA standards of safety and effectiveness. This means they can help protect your child’s teeth and mouth from injury when used as directed.
Prevention is the key to a healthy smile! Don’t wait to take your child to the dentist until pain or a dental emergency happens. Regular dental exams and professional cleanings can help your child have a lifetime of healthy smiles.
Read this information and keep it in a handy spot so you can quickly and calmly handle a dental emergency.
Knocked-out tooth — Go to the dentist right away. It’s best for your child to see a dentist within 30 minutes. Don’t forget to bring the tooth and any tooth pieces you can find!
Baby tooth (Primary) – It’s normal for children to lose baby teeth, but an accident that damages a primary tooth could also harm the permanent tooth underneath it.
Adult tooth (Permanent) – Unlike a baby tooth that is knocked out, an adult tooth should be put back into its socket (if possible).
Broken or cracked tooth — Go to the dentist right away, and bring the broken tooth piece with you (if possible).
Bitten cheek, tongue or lip
Object caught between teeth
Toothache or swollen face – Swelling of the face can be a sign of serious infection. If your child’s face is swollen, take your child to their dentist or physician.
Possible broken jaw – Apply a cold compress to control swelling. Take your child to the dentist or an urgent care center right away.
Knowing how to handle a dental emergency can make the difference between saving and losing your child’s tooth.
Read this page and then bookmark it so you can quickly and calmly handle a dental emergency.
Go to the dentist right away. It’s best to see a dentist within 30 minutes. Bring the tooth and any tooth pieces you can find.
It’s normal for children to lose baby teeth, but an accident that damages a primary tooth could also harm the permanent tooth underneath.
Swelling of the face can be a sign of serious infection. If your child’s face is swollen, take your child to your dentist or physician.
What is the focus of your child’s beautiful SMILE? Strong, healthy teeth!Baby teeth-also called primary teeth-are important in the growth and development of a child. Baby teeth can help your child chew foods and speak. They also hold space in the jaws for adult teeth that are growing under the gums. Babies are born without teeth. Usually baby teeth start to appear in the mouth when the child is 6 months old. By the third birthday, most children have a full set of 20 baby teeth including incisors, canines and molars. The chart below tells the names of baby teeth, when they come in (erupt) and when they fall out (are shed). Baby teeth be will replaced by permanent (adult) teeth. However, not all children get the same teeth at the same times. Your child’s teeth may erupt earlier or later than the times shown here.
Surprisingly, tooth decay can occur as soon as your child’s first tooth comes in (erupts). So it is very important to start taking care of those “pearly whites” as soon as you see them peeking through the gums. If your child gets decay, your child can suffer pain and infection. Also, if a child is in pain, he may have trouble eating, sleeping and learning.
 Decay in baby teeth
Decay in baby teethProtect your child’s teeth by starting dental checkups early. The American Dental Association and the American Academy of Pediatric Dentistry recommend that the first dental visit should occur when the baby’s first tooth appears, but no later than the child’s first birthday. Why schedule a visit so early? A dentist can show you how to clean your child’s teeth, talk about feeding, oral habits and recommend dental care products.
He or she also can help you make sure your child is getting the right amount of fluoride (FLOOR-ide), a natural mineral that protects teeth. And your dentist can answer questions about your baby’s teeth. Having a well-baby checkup at this age also connects your child to a dental home. This is a place where you can take your child from year to year. This helps the dentist get to know your child’s and family’s needs, so your child will have the best care. If your child is a toddler, the dentist will gently examine his or her teeth and gums, looking for decay and other problems. The dentist may also clean the child’s teeth. Your toddler can also be checked for problems related to habits such as thumb or finger sucking. Fluoride treatments and dental sealants are two important ways your dentist can prevent cavities. Dental sealants are a coating that the dentist puts on the grooves of your child’s back teeth to protect them. Your dentist will let you know if these treatments are right for your child.
Between the ages of 6 and 12, children go through a lot of changes. These include changes to their faces, teeth and jaws. Over time, your child’s baby teeth are replaced by adult teeth. A 6- to 12-year-old child has both baby and adult teeth. Together, they help children eat, speak and smile.
At about age 5 or 6, children begin to lose their bottom and top front teeth. By age 12, they will usually lose the last of their 20 baby teeth.
Their first adult, or permanent, teeth usually come in (erupt) between ages 6 and 7. The first adult teeth to come in are the molars, in the back of the mouth. They have flat surfaces that are especially good for chewing tough foods, like meat. It is important to take good care of them because they are meant to last a lifetime.
By the time your child is 12 to 14 years old, they usually have all of their adult teeth except their wisdom teeth. But, not all children get the same teeth at the same time. Your child’s teeth may erupt earlier or later than shown in the chart to the right.
A healthy diet that limits sugary beverages and snacks is good for overall well-being as well as for healthy teeth. A steady diet of sugary or acidic food and beverages can damage your child’s teeth. This includes 100% juice drinks, sports drinks, soda and energy drinks. Plaque on teeth turns the sugar in these drinks to acid. The acid attacks the hard surface of the teeth, known as enamel (e-NAM-uhl), and tooth decay and cavities can start to form. A cavity is a hole in the outer layer of enamel of the tooth. Cavities do not go away on their own, and must be treated by a dentist.
Having sugary beverages or snacks many times a day allows bacteria to make acid throughout the day. This increases the risk of getting cavities. To protect your child’s teeth from acid attacks and tooth decay, limit snacking between meals or offer nutritious options that are low in added sugar.
A dental sealant is a thin plastic coating that is put on the chewing surfaces of the back teeth. The sealant material flows into the pits and grooves on those surfaces and acts like a barrier, protecting enamel by “sealing out” bacteria and bits of food that can cause tooth decay.
Nine out of ten cavities children get are on their permanent back teeth. Sealants can help prevent most of these cavities.
Sealing a tooth is fast and painless. Sealants can last several years before they need to be reapplied. Ask your child’s dentist if sealants will help your child.
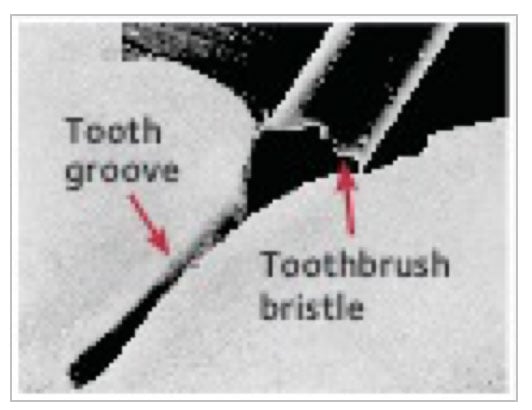
Even a toothbrush bristle is too big to reach inside a groove in the tooth (magnified).
Although most children can brush their own teeth by age 6, they should still be supervised until around age 10. This helps you make sure that they are cleaning their teeth the right way. Be sure your child uses short, gentle strokes to move the brush back and forth while cleaning all areas of the teeth: the outer surfaces, inner surfaces and chewing surfaces. Show your child how to place the toothbrush at a slight angle toward the gums when brushing along the gum line. Teach them to spit out all of the toothpaste after brushing.
By around age 10 or 11, most children should be able to brush their teeth without supervision. If you’re not sure if your child is ready, talk to their dentist or dental hygienist.
Cleaning between your child’s teeth daily helps remove plaque where toothbrush bristles can’t reach. Start using floss, a floss aid or another between-the-teeth cleaner when your child has 2 teeth that are next to each other. Your dentist or hygienist can show you and your child how to clean between the teeth.
Cleaning between their teeth may not be easy for children to do by themselves. The ADA recommends that you clean between your child’s teeth daily until they can do it alone, around age 10 or 11.
Look for the ADA Seal of Acceptance when choosing products like toothbrushes, toothpastes, floss and floss aids. The ADA Seal means that the products have been tested and shown to help keep mouths healthy.

By the time a child is 6, a dentist can check how well their teeth meet, known as their “bite.” A bad bite is when the teeth are crowded, crooked, or out of line, or the jaws don’t meet properly. A bad bite may be noticed as early as age 2, but it is usually seen between the ages of 6 and 12, when the adult teeth are starting to come in.
Early treatment may help prevent a bad bite or make it less severe. The dentist checks your child’s bite at every visit, which is another reason why regular dental appointments for children are important.
Fluoride (FLOOR-eyed) is a natural mineral that is found in all water sources — even the ocean. Fluoride helps protect tooth enamel from the acid attacks that cause tooth decay. It also helps repair weakened enamel before cavities form.
Children who drink tap water that has the recommended level of fluoride are less likely to get cavities than children who do not drink fluoridated water. If you are not sure if your tap water has fluoride, ask your dentist.
Children get added protection from fluoride by getting it from more than one source. Other sources of fluoride include fluoride toothpastes, fluoride mouthrinses and fluoride treatments applied in the dental office.
Many sports-related dental injuries can be prevented by wearing a mouthguard. Mouthguards usually cover the upper teeth and protect teeth, lips, tongue, face and jaw against injuries, so they should be worn in any activity where injury may occur, including non-contact activities like rollerblading and gymnastics.
The best mouthguard is one that fits properly and is worn regularly. Your dentist can make a custom mouthguard that fits your child’s mouth, is comfortable and protects the jaw. You can also purchase a ready-made mouthguard from a sporting goods store. If using a ready-made mouthguard, look for one that has the ADA Seal of Acceptance. Mouthguards that have earned the ADA Seal have been tested and proved to help protect the teeth and mouth from injury when used as directed.
Treating a sports-related dental injury can cost thousands of dollars, so a custom-made mouthguard for your child is an excellent investment!
Don’t wait to take your child to the dentist until pain or a dental emergency happens!
Regular dental exams and professional cleanings can help your child have a lifetime of healthy smiles.
Baby teeth, also called primary or deciduous (de-SID-joo-us) teeth, help your child chew and speak normally. They hold space in the jaws for the adult (permanent) teeth that come in later.
Your baby’s teeth usually start to appear in the mouth when the child is 6 months old. By age 3, most children have a full set of 20 baby teeth. Baby teeth will later be lost as your child grows, but if a baby tooth is lost too early, it may cause issues like crowding when the adult teeth come in.
Adult teeth begin to come in around age 6. By the time children are teenagers, they usually have all of their adult teeth.
The chart to the right shows when each tooth usually comes in (erupts) and is lost (shed). Not all children get the same teeth at the same time. Your child’s teeth may come in earlier or later than shown here.
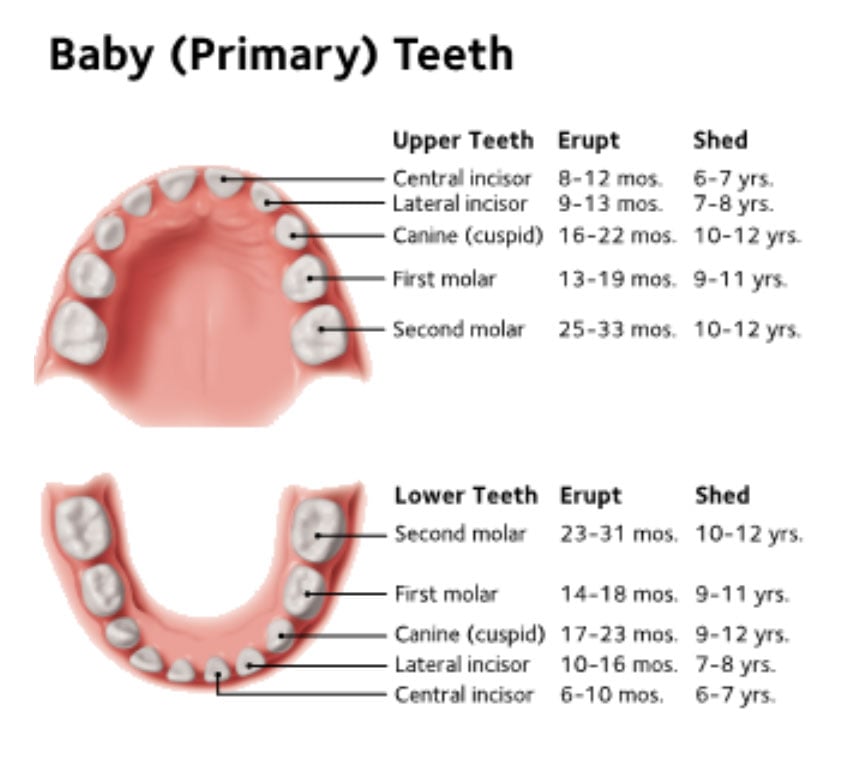
As teeth come in, babies may have sore or tender gums. When your baby is about 6 months old, you may want to start looking for signs of teething, like irritability, drooling more than usual and chewing or biting on hard items. Gums may swell and your baby may have a harder time sleeping or eating. To help your baby feel better, you can:
If your baby is still cranky and uncomfortable, talk to their dentist or pediatrician.
The U.S. Food and Drug Administration (FDA) warns parents not to use benzocaine-containing over-the-counter products to soothe sore gums in young children. These can include products such as Anbesol®, Hurricaine®, Orajel® and Orabase® and some prescription products. These products can cause serious reactions in children. Details are available on the FDA website: www.fda.gov.
Your baby should have their first visit with the dentist after their first tooth appears, but no later than their first birthday. This first visit is a “well-baby checkup” for your child’s teeth. It’s best for your child to have a pleasant first meeting with the dentist. Baby teeth can start to decay as soon as they come in, so forming good oral health habits early is important. Making sure your child is as comfortable as possible with their dentist will help them develop healthy habits. Don’t wait until an emergency comes up to introduce them to the dental office!
Sugar is in almost everything that a baby drinks, other than water. This can include 100% juices, breast milk and formula. Sugar left over from food and drink can turn into acid that can attack teeth. The acid can wear the hard outer surface of the teeth, called enamel (e-NAM-uhl), and tooth decay and cavities can start to form.
There are many steps you can take to help prevent decay and keep your baby’s teeth strong.
Breastfeeding:
Bottles, Sipping and Snacking:
Pacifiers:
Brushing and cleaning between the teeth is as essential for children as it is for adults. Brush your child’s teeth (and yours!) 2 times a day and for 2 minutes each time. You should clean between teeth with floss or a floss aid every day.
Brushing teeth the right way is important, so you should brush your child’s teeth until they have the skills to do it the right way on their own. Although most children can brush their own teeth by 6 years old, they should still be supervised until around age 10.
When you teach your child how to brush the right way, it may help to stand behind them and hold the brush while they watch in the mirror. Teach them to spit out all of the toothpaste after brushing.
Here are some tips for proper brushing:

For children under three years old.

For children three to six years old.
Cleaning between your child’s teeth with floss or another between-the-teeth cleaner removes plaque where toothbrush bristles can’t reach. Begin using floss or a floss aid when your child has 2 teeth that are next to each other. Flossing is not easy for children to do by themselves. The ADA recommends that you clean between your child’s teeth daily until they can do it alone, around age 10 or 11.

Healthy baby teeth

Moderate decay

Moderate to severe decay

Severe decay
Fluoride (FLOOR-eyed) is a mineral that is found in all natural sources of water — even the ocean. Fluoride helps protect tooth enamel from the acid attacks that cause tooth decay. It also helps repair weakened enamel before cavities form.
Children who drink tap water that has the recommended level of fluoride are less likely to get cavities than children who do not drink fluoridated water.
Children get added protection from fluoride by getting it from more than one source. Another source of fluoride, besides tap water, is fluoride toothpaste. Fluoride toothpaste is safe, even for young children, as long as they use the recommended amount of toothpaste and spit it out when they are done brushing. Children younger than 3 years old should use no more than a grain-of-rice sized amount of fluoride toothpaste. Children aged 3 to 6 years old should use a pea-sized amount of toothpaste. Fluoride mouth rinses are not recommended for children younger than 6.
Many infants and young children like to suck on thumbs, fingers and pacifiers. Sucking is a natural reflex and necessary for feeding. However, long-term sucking habits can cause problems. The child’s teeth may not grow in straight and his or her mouth may not develop correctly.
Sucking habits usually stop between the ages of 2 and 4. If your child uses a pacifier or sucks their fingers, talk to their dentist about how to get your child to stop this habit. If the sucking continues, ask your child’s dentist or pediatrician about other ways to discourage sucking.
Set up your child for a lifetime of healthy smiles by starting dental visits early. The American Academy of Pediatric Dentistry and the American Dental Association recommend that your child’s first visit to the dentist happens when their first tooth appears but no later than their first birthday. Baby teeth can start to decay as soon as they come in. It is important that your child is as comfortable as possible with their dentist so they develop healthy habits.
This first visit is a “well-baby checkup” for your child’s teeth. It’s best for your child to have a pleasant first meeting with the dentist. Don’t wait until pain or an emergency comes up to introduce them
to the dental office.
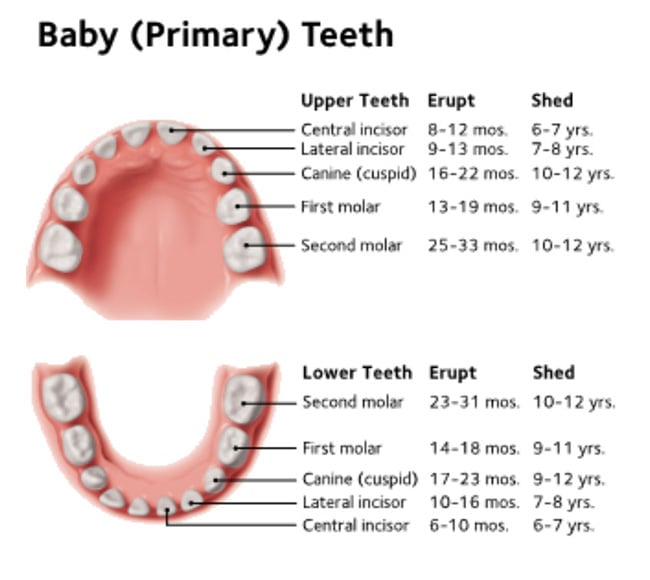
Baby teeth, also called primary or deciduous (de-SID-joo-us) teeth, usually start to appear in the mouth when a child is 6 months old. By their third birthday, most children have a full set of 20 baby teeth.
Baby teeth are important because they help your child to speak clearly and chew properly. They also hold space in the jaw and help form a path that adult (permanent) teeth can follow when it is time for them to come in. If a baby tooth is lost too early, it may cause issues like crowding when the adult teeth come in.
The chart below shows when baby teeth come in (erupt) and when they fall out (shed). Baby teeth will be replaced by adult teeth. However, not all children get the same teeth at the same times. Your child’s teeth may come in earlier or later than the times shown here.
Sugar is in almost everything that a baby drinks, other than water. This can include 100% juices, breast milk and formula. Sugar left over from food and drink can turn into acid that can attack teeth. The acid can wear the hard outer surface of the teeth, called enamel (e-NAM-uhl), and cavities can start to form. This is not only painful but it also can be dangerous. Cavities are caused by an infection, which can get worse and even make your child sick if they are not treated.
Decay can destroy baby teeth if it’s not treated.

Healthy baby teeth

Moderate decay

Moderate to severe decay

Severe decay
Don’t wait to take your child to the dentist until pain or a dental emergency happens. Regular dental exams and professional cleanings can help your child have a lifetime of healthy smiles.
If you have missing teeth, a removable partial denture is one way to replace them. These are a few of the advantages of a removable partial denture:
When you lose a tooth, the nearby teeth may tilt or drift into the empty space. The teeth in your other jaw may also shift into the space. This can affect your bite and place more stress and wear on your teeth and jaws. You may find it harder to clean teeth that have shifted, which can lead to tooth decay and gum disease. This is why it’s important to replace missing teeth.
When teeth are lost and not replaced, the face looks older. The lips appear thin and flattened. The chin moves forward and upward and appears pointed.
Also, the mouth loses some of its shape, and the lip line straightens. Pouches become pronounced on either side of the lower jaw. Cracks and sores may form at the corners of the mouth.
A removable partial denture usually has replacement teeth attached to a metal or acrylic (plastic) base that matches the color of your gums. Partial dentures often have some form of clasp that attaches to your natural teeth and can easily be taken out of your mouth for cleaning or storing while you sleep.
Your dentist may also recommend crowns, or “caps,” on your natural teeth to improve the way a removable partial denture fits your mouth.
It takes practice to put in and take out a removable partial denture. It may feel a bit odd or tight for the first few weeks. But in time, you will get used to it. Never force the denture into place by biting down. This could bend or break the clasps or damage your teeth. Your dentist will show you how to place and remove it.
Your dentist may tell you to take out the partial denture at bedtime and put it back in when you wake up. Usually your dentist will make follow-up appointments to look for pressure points or sore spots. They will also adjust your partial denture so that it fits comfortably.
When you replace missing teeth, eating is much easier. But, it takes practice.
If you have missing teeth, wearing a removable partial denture can help you speak more clearly. If you find that some words are hard to say at first, try reading out loud in front of a mirror. With time and practice, you should be able to speak well.
Like natural teeth, you must take good care of your removable partial denture. Here are some tips:
This removable partial denture replaces 6 missing teeth and attaches to the natural teeth with metal clasps. It can be removed for easy care and cleaning.
As you get older, the fit of your removable partial denture can change. Your jaw bone can shrink, making a space under the denture. Food can get trapped. The denture clasps also may get loose from normal wear.
If your partial denture needs adjusting, do not try to adjust it yourself. You can harm both the denture and your mouth. And, don’t use household glues to repair it because they can contain harmful chemicals.
If your removable partial denture breaks, cracks, or chips, or if one of its teeth become loose, see your dentist as soon as possible. Also, your partial denture may need to be adjusted if you lose one of your supporting natural teeth. Sometimes dentists can make the repairs, often on the same day. Complex repairs can take longer. The sooner you make an appointment, the sooner you can have a well-fitting partial denture again.
Your dentist will tell you how often to schedule dental visits. Regular exams and professional cleanings are very important to keep your smile healthy.
Mouth sores can be painful, annoying and unsightly.
Some appear inside the mouth – on the gums, tongue, lips, cheeks or palate (roof of the mouth). Others, like cold sores, can appear outside the mouth, such as on and around the lips, under the nose and on the chin.
Although there are many types of mouth sores, the most common are canker sores, cold sores, leukoplakia (a thick white or gray patch) and candidiasis or thrush (a fungal infection).
Some people may experience occasional discolored, painless spots in their mouth. Most are harmless and will disappear or remain unchanged. However, some sores or spots can be serious and need the attention of your dentist or physician. For example, oral cancer may not be painful at first, but it can be deadly. That’s why regular dental checkups are important. Have your dentist examine any mouth sore or spot that fails to heal within two weeks.

The exact cause of canker sores is not known. Genetics play a role. White cells (lymphocytes) in our immune system may affect the lining of the mouth causing these irritating, but harmless, sores. Fatigue, emotional stress, and certain foods can increase the possibility of a canker sore for some people. Even biting the inside of the cheek or tongue or chewing a sharp piece of food may trigger a canker sore.
Canker sores are not contagious or precancerous. There is no permanent cure for canker sores; therefore, treatment is for discomfort or pain. Over-the-counter topical medications (such as numbing agents or protective ointments) and antimicrobial (germ-fighting) mouth rinses may offer temporary relief. Avoid hot, spicy or acidic foods and beverages that can irritate the sore. Treatment for an attack involves corticosteroids, Prednisone-like medications that control troublesome lymphocytes. The medication may be in a topical form (applied to the skin), or systemic (taken as a tablet or capsule).
 Cold sores are groups of painful, fluid-filled blisters (often called fever blisters). These unsightly sores usually erupt on the lips, and sometimes on skin around the lips. Clusters of small blisters may also occur on the gum tissue near the teeth and/or on the bony roof of the mouth.
Cold sores are groups of painful, fluid-filled blisters (often called fever blisters). These unsightly sores usually erupt on the lips, and sometimes on skin around the lips. Clusters of small blisters may also occur on the gum tissue near the teeth and/or on the bony roof of the mouth.
Cold sores – caused by herpes virus Type 1 or Type 2 – are contagious. The initial infection (primary herpes), which often occurs before adulthood, may be confused with a cold or the flu. The infection can cause painful lesions to erupt throughout the mouth, and some patients can be quite ill for a week. Most people who get infected with herpes do not get sick, however. Once a person is infected with herpes, the virus stays in the body, where it may remain inactive. Unfortunately, in some people, the virus becomes activated periodically, causing the cold sore to appear on the lips or other sites. A variety of irritants (wind, sun, fever, stress) can cause a flare.
Cold sores usually heal in about a week. Once the blister breaks, an unsightly scab forms. Over-the-counter topical anesthetics and protectants, anti-inflammatory agents or topical antiviral agents may provide temporary relief for the discomfort but do little to speed healing. As with the common cold, there is no cure for these viral infections. Topical or systemic antiviral drugs can be prescribed by your dentist, but they are ineffective after 3 to 4 days of blister formation and usually are not recommended in otherwise healthy patients.
 Leukoplakia (loo-koh-PLAY-kee-ah) is a white or gray patch that develops anywhere on the inside of the mouth. It is caused by excess cell growth of the lining of the mouth. It is often a response to chronic irritation, such as smoking or smokeless tobacco (snuff, chewing tobacco), certain foods, cheek biting, irregular dental restorations or broken teeth. In some instances, a cause cannot be determined. Leukoplakia patches develop slowly over a period of time. The patch may eventually become rough. It typically is not sensitive or painful.
Leukoplakia (loo-koh-PLAY-kee-ah) is a white or gray patch that develops anywhere on the inside of the mouth. It is caused by excess cell growth of the lining of the mouth. It is often a response to chronic irritation, such as smoking or smokeless tobacco (snuff, chewing tobacco), certain foods, cheek biting, irregular dental restorations or broken teeth. In some instances, a cause cannot be determined. Leukoplakia patches develop slowly over a period of time. The patch may eventually become rough. It typically is not sensitive or painful.
Leukoplakia generally is harmless, but there is a risk that it can become cancerous. To be certain that a spot or sore is not a threat, your dentist may do a biopsy to determine if any potentially dangerous cells are present. If the leukoplakia is sensitive, cancer must be ruled out by biopsy.
 Erythroplakia (e-ryth-ro-PLAY-ki-a) is a red patch that may be found in any part of the mouth but is most common in the floor of the mouth or on the gum tissue behind the back teeth. The cause is unknown but is most likely associated with smoking or other tobacco use and alcoholic beverages. Chronic irritation and poor nutrition may also be contributing factors. Although erythroplakia is less common than leukoplakia, most of these lesions are found to be precancerous or cancerous when biopsied. Red lesions that do not heal in a week or two should be evaluated by your dentist. This applies even if you do not smoke or drink alcohol.
Erythroplakia (e-ryth-ro-PLAY-ki-a) is a red patch that may be found in any part of the mouth but is most common in the floor of the mouth or on the gum tissue behind the back teeth. The cause is unknown but is most likely associated with smoking or other tobacco use and alcoholic beverages. Chronic irritation and poor nutrition may also be contributing factors. Although erythroplakia is less common than leukoplakia, most of these lesions are found to be precancerous or cancerous when biopsied. Red lesions that do not heal in a week or two should be evaluated by your dentist. This applies even if you do not smoke or drink alcohol.
 Lichen planus (li-ken PLAY-nus) is a disorder that involves a chronic, itchy, inflammatory rash or lesion on the skin or in the mouth. The lesions may consist of white spots or “lacelike” white changes. Lesions on the sides of the tongue, insides of the cheek and on the gums, may be tender or painful. Its cause is genetic and related to a chronic immune system reaction.
Lichen planus (li-ken PLAY-nus) is a disorder that involves a chronic, itchy, inflammatory rash or lesion on the skin or in the mouth. The lesions may consist of white spots or “lacelike” white changes. Lesions on the sides of the tongue, insides of the cheek and on the gums, may be tender or painful. Its cause is genetic and related to a chronic immune system reaction.
Lichen planus generally occurs during or after middle age. Lichen planus is not contagious and does not pose a high risk for becoming cancer. There is no cure, so treatment is for discomfort or pain. Rinses, ointments, or pills can be prescribed by your dentist, if needed. The diagnosis can be confirmed by biopsy and clinical characteristics.
 Candidiasis (can-di-DI-a-sis), also known as oral thrush or moniliasis, is a fungal infection. It produces creamy white and red patches that form on surfaces of the mouth. It can be painful and may cause bad breath and difficulty tasting and/or swallowing.
Candidiasis (can-di-DI-a-sis), also known as oral thrush or moniliasis, is a fungal infection. It produces creamy white and red patches that form on surfaces of the mouth. It can be painful and may cause bad breath and difficulty tasting and/or swallowing.
It occurs when the yeast Candida albicans reproduce in abnormally large numbers. For example, Candida may flourish after antibiotic treatment, when normal bacteria in the mouth have decreased, when the immune system is suppressed or when the mouth is dry (xerostomia). Dry mouth is a common side effect of many prescription or over-the-counter medications.
Candidiasis most often occurs in the very young, the elderly, and those debilitated by disease, such as diabetes and AIDS. It also frequently occurs among people who wear dentures.
Treatment consists of controlling conditions that cause the outbreak. Cleaning dentures to remove Candida is important in preventing denture-induced problems.
Saliva substitutes or prescription medications are also available to treat dry mouth. Antifungal medications may be used when the underlying cause cannot be treated or eliminated. Good oral hygiene is essential.
Oral or mouth cancer may appear on the lips, tongue, cheek lining, gums, palate (roof of the mouth) or floor of the mouth. Cigarettes and other tobacco products, including smokeless tobacco, are associated with 70 percent of oral cancer cases. Drinking alcoholic beverages can also increase your chances of having oral cancer.
Oral cancer may appear as a white or red lesion, lump or ulcer. It is usually small and painless at first, but can grow and spread quickly. Many oral cancers are discovered during routine dental examinations. Control of leukoplakia and erythroplakia may prevent some oral cancers from developing. Some oral cancers can resemble benign (non-dangerous) changes, so may delay early diagnosis. Early diagnosis and treatment increase the chance of a good quality of life.
Do you sip soft drinks or other sugary drinks all day at your desk? Do you use breath mints or eat candy often? Instead of eating meals, do you snack all day? Do you often grab a sports or energy drink when you are tired?
If you answered yes to any of these questions, you may be increasing your chances of tooth decay. Keep reading to find out why.
 Eating habits and food choices can lead to tooth decay, or cavities. A steady supply of sugary foods and drinks, including sports and energy drinks, can damage teeth. But snacking or “grazing” all day long can also lead to tooth decay.
Eating habits and food choices can lead to tooth decay, or cavities. A steady supply of sugary foods and drinks, including sports and energy drinks, can damage teeth. But snacking or “grazing” all day long can also lead to tooth decay.
Plaque (sounds like “back”) is a sticky film of bacteria that forms on teeth. When you do not remove plaque from your teeth every day, it builds up. Plaque bacteria use sugar to make acid that attacks enamel, the hard surface of the tooth. The acid can attack tooth enamel for up to 20 minutes after you consume sugary foods or drinks.
When you have sugary foods or drinks many times a day or sip the same sugary drink for a long time, acid attacks the enamel again and again. Repeated acid attacks can cause tooth decay, which must be treated by a dentist.
One way of making smarter food and drink choices is to read their labels to make sure they are low in added sugar.
Eating a healthy diet helps keep you from feeling tired, getting sick, being overweight, and having other health problems, like tooth decay. A healthy diet is one that
Almost all foods have some type of sugar. You cannot and should not remove all sugar from your diet. Many foods and drinks, like apples, carrots, and milk, naturally contain sugars and have vitamins, minerals, and nutrients that your body needs.
For teeth to be healthy, they need vitamins, protein, calcium, and phosphorous.
 Chew sugarless gum that has the ADA Seal. Chewing gum for 20 minutes after meals has been shown to reduce tooth decay.
Chew sugarless gum that has the ADA Seal. Chewing gum for 20 minutes after meals has been shown to reduce tooth decay.Look in the mirror.
If your answers show that you might want a change in your smile, talk to your dentist about Improving Your Smile.
A great smile can be the most attractive feature of your face. A smile helps you express health, success, youth and sincerity. It is a great asset in your personal, business and social contacts. So it’s important that you are happy with how your smile looks. But if you are like many people, you may not be.
Your dentist has many different techniques to shape, sculpt, and make your smile more beautiful. With a few simple steps, you can have a smile you feel great about. And treatment may be more affordable than you think.
Example of an Improved Smile


Your dentist can use natural-colored materials to restore teeth that have cavities. Options include composite materials, such as resin, as well as lab-made porcelain inlays, inlays and crowns.
Teeth become stained for many reasons – drinking coffee, tea or wine; smoking; and even aging can discolor teeth. Tooth whitening is a process that makes discolored teeth whiter. The bleach used for in-office (chair side) whitening is stronger than the bleach found in at-home whitening kits. Keep in mind that not everyone’s teeth can become movie-star white. Your dentist can recommend the whitening treatment that is right for you.
Veneers are thin, tooth-colored shells that are bonded, or cemented, to the front of your teeth. They are custom-made of ceramic or composite resin, and look like natural teeth. Veneers can be used to fill spaces between teeth and to cover teeth that are stained, poorly shaped, or a bit crooked.
Braces can help correct crowded or crooked teeth or an uneven bite. Braces have become much smaller and less noticeable over the years. Brackets, the part of the braces that attach to each tooth, can sometimes be attached to the back of the tooth to make them less noticeable. Some brackets are clear or tooth coloured-which help braces blend in.
In some cases, treatment may be done without using braces at all. A series of clear, removable aligners are used to move your teeth over time. These aligners are more discreet than traditional braces.
Your dentist can “reshape” your teeth by contouring tooth enamel, the outer layer of the tooth. When teeth are a little crowded or uneven, or when teeth appear too long, your dentist can use enamel shaping to improve how the teeth look.
If a tooth needs more a dramatic change than veneers or enamel shaping can provide, crowns are an option. The outer part of the tooth is removed and a crown is placed over it. The crown can be made to fit in with your other teeth. It’s like a fresh start for your tooth.
Once you decide to improve your smile, the first step is to visit your dentist. At this visit, you will talk about the best plan for you. If you have any signs of dental disease, your dentist may recommend treatment for this. It’s important to have a healthy mouth before starting cosmetic treatment.
These treatments and others can help you have more natural-looking and attractive teeth. What are you waiting for? Talk to your dentist today about how to make your smile the best it can be.
Oropharyngeal cancer can be hard to spot because it develops in places that are hard to see. Signs and symptoms to look out for include:
If any of these symptoms last for more than two weeks, let your dentist know.
It is estimated that HPV causes approximately 70 percent of oropharyngeal cancer. The number of cases of oropharyngeal cancers caused by HPV is on the rise. For example, according to a report from the Department of Health and Human Services (HHS), the number of HPV-related throat cancer cases doubled from 1999–2015 (Figure), with the greatest increase seen among men.
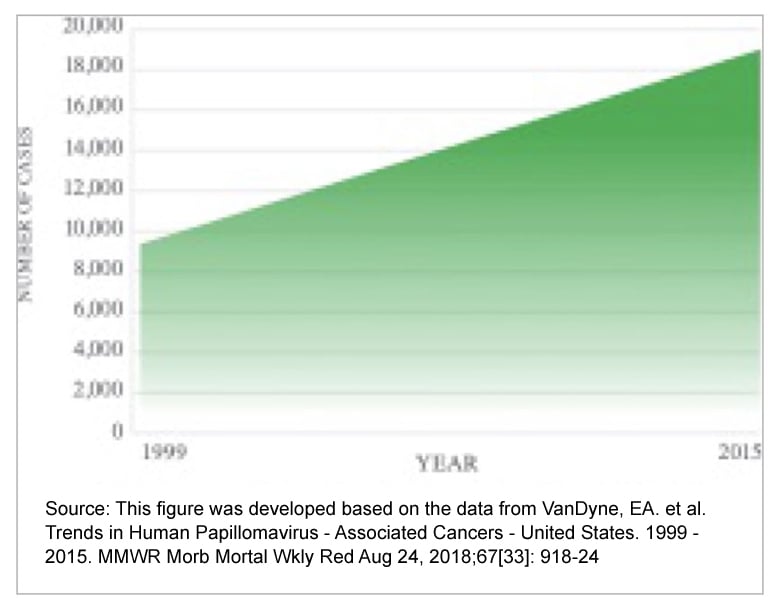
Infection with the human papillomavirus (HPV) is very common. It is estimated that more than 8 out of 10 adults have been infected with HPV by the time they are 45 years old. Most of the time, HPV infections clear up without causing any problems. But, sometimes the virus stays in the body and may cause cancer later in life.
HPV vaccination is the best way to prevent HPV infections. The HPV vaccine helps protect against infection from a virus that may lead to cancer.
HPV is a leading cause of oropharyngeal (or-oh-FARE-in-jee-al) cancer. Oropharyngeal cancer is a type of head and neck cancer that develops near the back of the mouth and throat (Figure), in places like the
The HPV vaccine was first offered to girls in 2006, and since that time, there has been a significant drop in HPV infections among teenage girls. Now offered to both boys and girls, experts say the HPV vaccine could prevent nearly 90 percent of HPV-related cancers in the United States.
HPV-related cancers develop years after a person is infected with the virus. Getting the vaccination as young as recommended is the best way to protect against the virus. The HPV vaccination can help protect older children and some adults, though an additional dose might be needed (Table).
The CDC recommends that
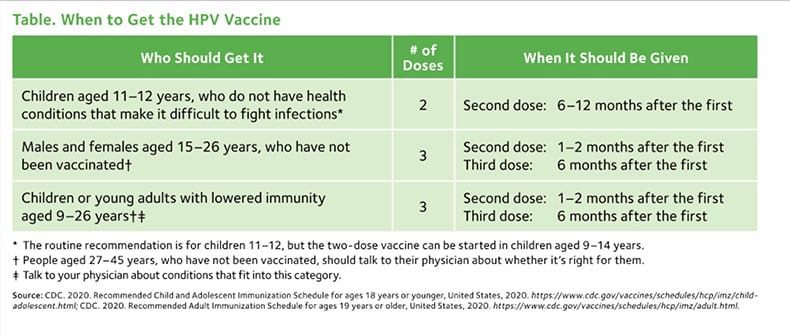
Experts say the HPV vaccine could prevent nearly 90 percent of HPV-related cancers in the United States.
Dental treatment is safe for pregnant women, according to the American Dental Association (ADA), the American College of Obstetricians and Gynecologists and the American Pregnancy Association. Preventive dental cleanings and annual exams are recommended during pregnancy because if dental disease is present and is not treated, it can lead to more serious health problems such as infection, pain and inability to eat. Delaying treatment until after your pregnancy may make any existing dental issues worse.
X-rays using proper shielding, giving local anesthesia and necessary emergency treatments, like a tooth extraction or root canal therapy, can all be performed safely by your dentist during pregnancy.
Your dentist is part of your healthcare team.
Be sure to tell your dentist if you:
If you are pregnant, make sure to tell your dentist and let him or her know when the expected delivery date is. This will help the two of you plan any necessary treatments before the baby arrives.
Your dentist can talk with your physician or OB/GYN about any treatment that is recommended. If you are planning to become pregnant, have your teeth professionally cleaned at your dentist’s office and schedule any needed treatment. This can help lower your risk of having a dental emergency during your pregnancy.
There are many medications that are safe to have during pregnancy, including local anesthetics and some antibiotics. Your dentist may talk with your physician to determine which medicines — such as pain relievers — you may take safely during your pregnancy. Discuss any questions or concerns you have with your dentist and physician.
Routine dental x-rays during pregnancy are generally safe. Radiation from dental x-rays is very low, and your dentist may cover your abdomen with a protective shield (lead apron). If an x-ray exam is needed, your dentist will discuss this with you and take steps to reduce your radiation exposure.
Many women develop gingivitis (jin-ji-VY-tis) during pregnancy. The hormonal changes during pregnancy can make your gums more sensitive to plaque. Your gums may become red and tender and may bleed easily when you brush your teeth. If gingivitis is not treated, it may lead to more serious gum diseases. Your dentist may recommend more frequent professional cleanings to help you avoid problems.
Dental caries (tooth decay) and tooth erosion may occur due to vomiting from morning sickness. Tooth decay may also develop because of changes in diet, like more frequent snacking, more acid in the mouth from dry mouth that sometimes occurs with pregnancy or poor oral hygiene habits.
In some women, growths of tissue called pregnancy tumors appear on the gums, most often during the second trimester. These growths or swellings are usually found between the teeth. Excess plaque can inflame the gums and cause them to swell. They bleed easily and appear red and shiny.
These growths may go away after your baby is born. If necessary, your dentist can remove them. If you notice any swelling or other changes in your gums, see your dentist.
Many pregnant women develop gingivitis, the early stage of gum disease. Signs of gingivitis include red and tender or swollen gums. They may bleed easily when you brush your teeth.
Pregnancy tumors may go away after your baby is born; if necessary, your dentist can remove them.
It’s important for your own health as well as your child’s to have a healthy mouth before your child is born. A wide variety of bacteria live in your mouth, which is normal. The film of bacteria on your teeth (called plaque) turns sugars in the foods you eat into acid that attacks the teeth. This can cause tooth decay and a cavity can form.
To help prevent tooth decay:

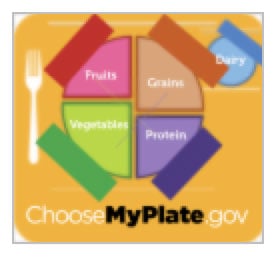
What you eat during pregnancy affects the growth of your developing baby — including their teeth. Your baby’s teeth begin to develop between months 3 and 6 of pregnancy. So, it’s important that you take in enough nutrients, especially calcium, protein, phosphorous and vitamins A, C and D.
You do not lose calcium from your teeth during pregnancy. Your diet — not your teeth — provides the calcium your baby needs. Be sure to get enough calcium in your diet for you and your baby by having at least 3 servings of dairy products or other calcium-rich foods each day. Or, your obstetrician (OB/GYN) may recommend that you take calcium supplements.
For more ideas about how to eat healthy, visit www.choosemyplate.gov.
Using any form of tobacco is not only harmful to your health, but it can also harm your developing baby. Not only does tobacco increase your risk of gum disease and cancer, but it also contains the highly addictive chemical, nicotine. Your newborn baby can be fussy and irritable because they are going through nicotine withdrawal. Smoking cigarettes while you are pregnant can increase your baby’s risk of low birth weight and developing chronic health problems like asthma. Talk to your dentist or physician about ways you can safely quit.
For more information about taking care of your mouth and teeth, visit MouthHealthy.org, the ADA’s website just for patients.
Talk to your dentist about snoring
Snoring happens when the muscles in your mouth and/or throat relax and cause your tongue or other soft tissues to block your airway when you’re sleeping. This makes it harder to breathe normally on your own. As you breathe in and out, you make a “snoring” sound when air tries to force its way through your blocked airway.
If you snore, then you probably already know that it can be an annoying distraction for your bedtime partner. But, snoring could also be a sign of a common sleep-related breathing disorder called sleep apnea (AP-nee-yuh). Sleep apnea occurs when your breathing slows down or stops one or more times when you are sleeping.
This causes your brain to wake your body up so that you can take in a deeper breath and get the right amount of oxygen. You may also take shallow or short breaths while you sleep. This cycle can repeat dozens or even hundreds of times each night. Over time, this can put a lot of physical stress on your body and can lead to serious health problems if it’s not treated — like heart disease or diabetes.
Talk to your dentist or physician if you:
These are some of the most common reasons why people may be affected:
Biology: Enlarged tonsils, a large tongue, or a small or misaligned jaw can raise your risk
of sleep apnea.
Being overweight/obese: Extra weight puts more stress on your body and makes it even harder to breathe normally when you sleep.
Genetics/family history: If other members of your family have sleep apnea, then you
may be affected by it, too.
Men are more affected than women, but it can also occur in women, especially after menopause.
Smoking and/or drinking alcohol affect your tongue and tissues in your mouth and throat, making it harder to keep your airway open when you sleep.
It’s important that you talk to your primary physician or a doctor who specializes in sleep medicine for an accurate diagnosis of sleep apnea. Then, your dentist can work with them to create a treatment plan that will help improve your quality of sleep and overall health. Treatment options range based on the severity of your sleep apnea.
Snoring is a common sign of sleep apnea, but not everyone who snores has sleep apnea. The best way to know for certain is to talk to your physician or a doctor who specializes in sleep medicine.
Pros: It’s shown to be the most effective way to control sleep apnea.
Cons: The machine can be loud and the mask may feel bulky when trying to sleep, which may make it difficult to use regularly.
Pros: More comfortable to wear and easier than a CPAP device to stick to using every night.
Cons: May not be effective in treating severe cases of sleep apnea.
Tobacco in any form is bad for your health
You are probably aware that tobacco may cause cancer, stroke and heart disease, but did you know that it can also cause serious harm to your mouth?
It doesn’t matter how you use it — whether you smoke, vape, dip or chew — tobacco is not good for you. Talk with your dentist or physician about ways to quit.
Smoking traditional tobacco products like cigarettes, pipes and cigars may cause serious health issues to your mouth and throat. Cigarette smoke has more than 7,000 chemicals and chemical compounds, like carbon monoxide and arsenic. At least 70 of them are known to cause cancer, including mouth or throat cancer.
Smoking is also linked to:
Overall, tobacco can negatively affect all parts of your health, including your mouth. It can lead to gum disease and tooth loss. Your teeth and tongue can become brown and stained. You can also have bad breath that doesn’t go away and can get mouth sores. Using tobacco also slows down healing after dental treatments.
Many people are turning to e-cigarettes and vaping devices because they believe they are a safer and healthier choice than traditional tobacco products. But, there is no current evidence to show that e-cigarettes and vaping devices are any safer than regular tobacco products.
The same toxic ingredients that are in cigarettes have also been found in the vapor of e-cigarettes. There are thousands of brands and types of vaping liquids on the market and there is little regulation on the levels of carcinogens. They all have different ingredients and different amounts of nicotine in them, so there isn’t a clear way to know what chemicals and how much nicotine you are inhaling every time you vape.
If you are addicted to nicotine, it will be difficult to stop using e-cigarettes.
According to the Centers for Disease Control (CDC), from 2017 to 2018, e-cigarette use went up 78% among high school students and 48% among middle school students.
Smokeless tobacco (also called chewing tobacco, spit, dip, snuff, snus or chew) contains more than 3,000 chemicals, including at least 28 cancer-causing ingredients. You may think that “smokeless” means “harmless,” but this is not true. Any kind of tobacco can harm your health.
In fact, if you use smokeless tobacco, you can take in a large amount of nicotine and cancer-causing chemicals without even lighting up.
The nicotine in smokeless tobacco is swallowed or absorbed through blood vessels in your mouth. Holding an average-sized dip in your mouth for 30 minutes gives you as much nicotine as smoking three cigarettes, making it very addictive and hard to quit.
Did You Know? American teens and tweens who use e-cigarettes are more than 4 times as likely to try a regular cigarette compared to those who never tried e-cigarettes.
Smoking waterpipes, or hookahs, has been linked to many of the same health problems as smoking cigarettes. They also pack a tobacco punch. A hookah smoking session could last as long as 60 minutes.
There are many types of hookah tobacco available, so you can’t know how much nicotine and other dangerous chemicals are in it every time you smoke. Water filtration does not limit the harmful effects of tobacco.
Did You Know? According to the CDC, a person puffs on a cigarette an average of 20 times, but they may take 200 puffs during an hour-long hookah session.
Children need strong, healthy teeth to chew their food, speak, and smile. Your child’s teeth also help give their face its shape and keep space in the jaw for their adult teeth to come in properly. Your child’s baby’s teeth start to come in when they are about 6 months old. Baby teeth will later be lost one by one. This makes space for adult teeth. By the age of 21, a person usually has all of their adult teeth. The last 4 teeth that come in are the wisdom teeth.
The charts below tell the names of the baby and adult teeth. The pictures show when each tooth usually comes in (erupt) and is lost (shed). But not all children get the same teeth at the same times. Your child’s teeth may come in earlier or later than the ages in these charts.
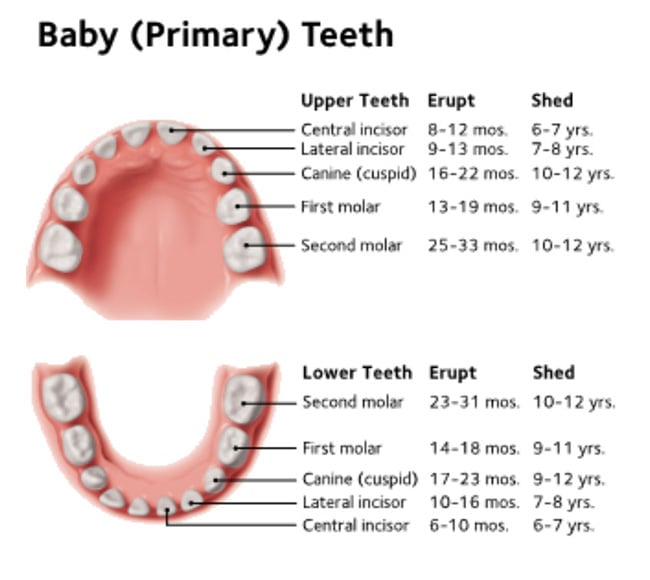
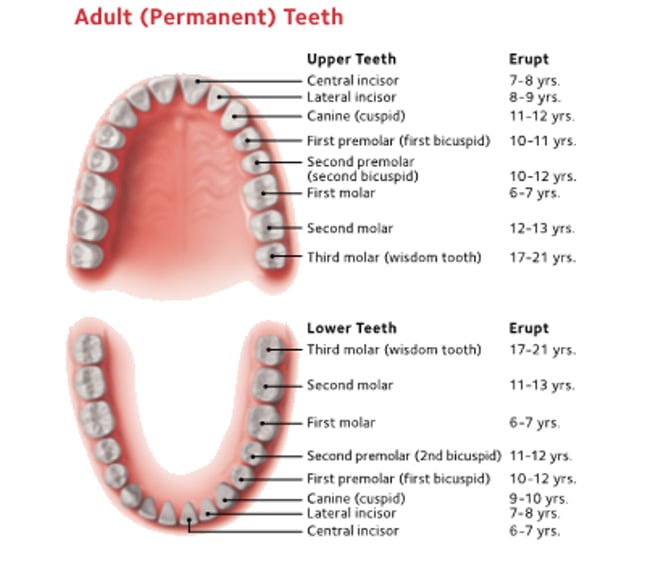
Most children go through a stage when they have mixed dentition. This means that they have a mix of baby and adult teeth. During this time their smile can look uneven, with some big teeth, some small teeth, some crowded teeth, or maybe even some missing teeth. Smiles often even out once all their adult teeth are in place.
When your child is around age 7, the dentist will do a dental “growth and development check” to make sure your child’s adult teeth are coming in properly and that the back teeth are working together the way they should. Your dentist may also take an X-ray of their teeth. If your child’s teeth or bite need treatment, it’s best to get an early start.
Adult teeth start to form under the baby teeth. After the baby teeth are lost, the adult teeth will come in through the gums.
Baby teeth are just as important as adult teeth. Baby teeth (also called primary teeth) help your child chew and speak. They also give the face its shape and hold space for adult teeth to come in the right way. That’s why it’s smart to take good care of baby teeth.
When your baby is born, they already have 20 baby teeth hidden in their jaws. Your baby’s first tooth begins to come in (or “erupt”) as early as 6 months after birth. The front 2 upper and 2 lower teeth usually appear first.
Most children have a full set of 20 baby teeth by the time they are 3 years old. As your child grows, their jaws also grow to make room for their adult teeth. By the age of 5 or 6, their adult teeth begin to erupt.
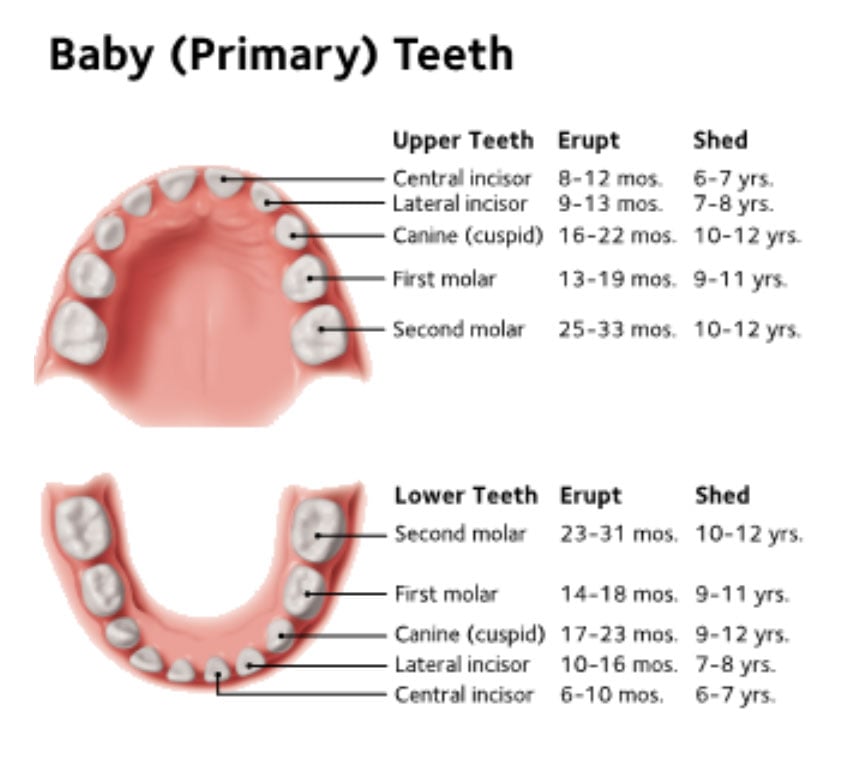
Sometimes a baby tooth is lost before the adult (permanent) tooth beneath it is ready to come in. If a baby tooth is lost too early, nearby teeth can shift into the open space. And when the adult tooth is ready to come into the space, there may not be enough room. The new tooth may be unable to come in. Or, it may erupt crooked or in the wrong place.
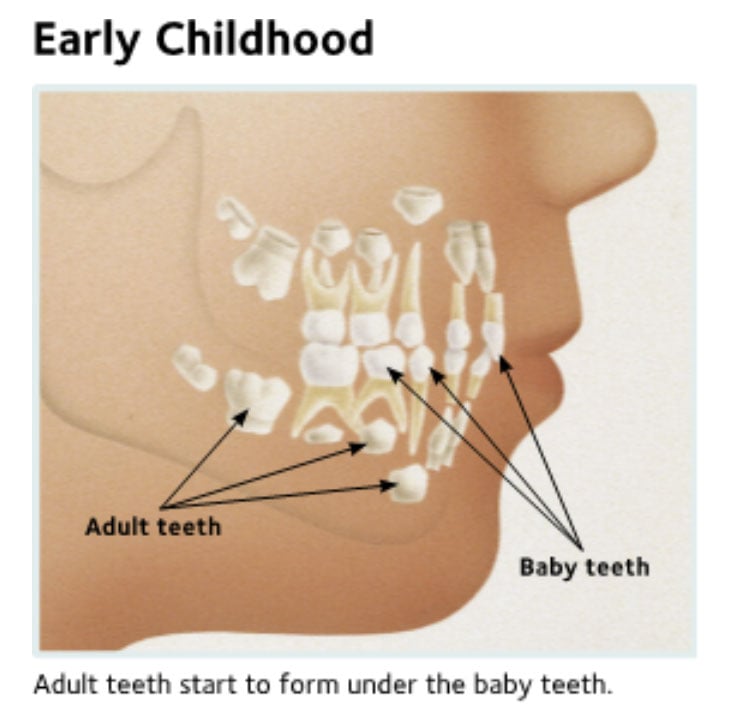
If your child loses a tooth early, the dentist may recommend a space maintainer. This is a plastic or metal piece that holds open the space left by the missing tooth. The dentist will remove this plastic or metal piece once the adult tooth begins to appear.
Tooth decay in baby teeth can affect the growth of adult teeth. It also can be painful. Your child may avoid eating and speaking normally if they have tooth pain, so it is important to take good care of baby teeth even though they will fall out later.
Decay can start as soon as teeth appear in your child’s mouth. Decay happens when baby teeth are in contact for long periods with liquids that have sugar in them. These liquids include sweetened water, soda, fruit juice, and even milk or formula.
Tooth decay can happen when you put your baby to bed with a bottle or use bottles to soothe them if they are fussy. Once your baby has started to eat solid foods, they may be given a bottle of water at these times.
Decay in Baby Teeth

Healthy baby teeth

Moderate decay

Moderate to severe decay

Severe decay

For children under three years old.

For children three to six years old.

Plan your child’s first dental visit after the first tooth appears, but no later than their first birthday. Consider it a “well-baby checkup” for your child’s teeth.
Contact us for an appointment
2467 S 17th Street Unit B
Wilmington, NC 28401
2467 S 17th Street Unit B
Wilmington, NC 28401
10 am – 6 pm
10 am – 6 pm
10am – 2pm
© City Dental. All rights reserved.
© City Dental. Content, including images, displayed on this website is protected by copyright laws. Downloading, republication, retransmission or reproduction of content on this website is strictly prohibited.